Evaluation of routine contouring of the pharyngeal constrictor muscles
Camilla Grindeland Boer,
Norway
MO-0645
Abstract
Evaluation of routine contouring of the pharyngeal constrictor muscles
Authors: Grete May Engeseth1,2, Camilla Grindeland Boer1, Vegard Vingelsgård1, Liv Bolstad Hysing1,3
1Haukeland University Hospital, Department of Oncology and Medical Physics, Bergen, Norway; 2The University of Bergen, Department of Clinical Science, Bergen, Norway; 3The University of Bergen, Department of Physics and Technology, Bergen, Norway
Show Affiliations
Hide Affiliations
Purpose or Objective
Late radiation
induced side effects like swallowing dysfunction are frequently reported by
patients treated for head and neck cancers (HNC). The dose to the pharyngeal
constrictor muscles (PCM) is considered a prognostic factor and it is
recommended to reduce PCM dose during treatment planning as much as possible. However,
contouring of PCM are time consuming, the purpose of this study was therefore to
evaluate the potential benefit of routine contouring and dose constraining of
the PCM in terms of reduction in dose and estimated Normal Tissue Complication
Probabilities (NTCP).
Material and Methods
The
patient material consisted of 30 patients with HNC in the oral cavity,
oropharynx and hypopharynx. Patients was was treated using VMAT with
simultaneously integrated boost. Prescribed dose were 68 Gy, 60 Gy and 50 Gy delivered in 6 fractions per week. In 15 of the patients the PCM were contoured during
treatment planning according to international consensus guidelines by
dedicated RTTs who were certified in OAR contouring after completion of an
in-house developed training program (Radiotherapy and Oncology (2015), 117 ; 83-90) . As dose constraint, the mean dose (Dmean)
to PCM ≤ 55
Gy was used as a starting point in the plan optimization; PCM dose was further
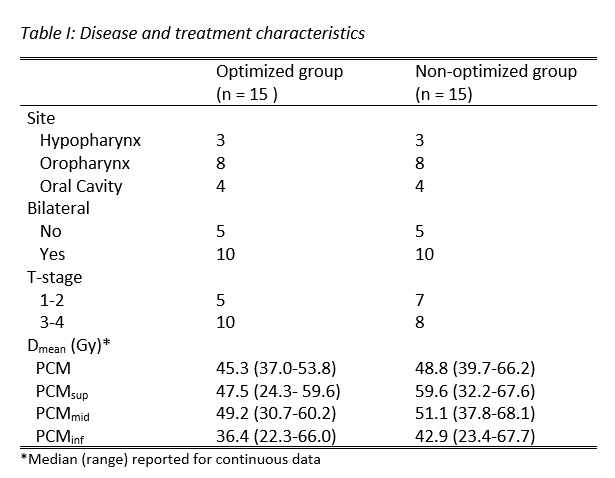
reduced if possible without compromising target dose coverage. Propensity
score matching using disease site, bilateral treatment and T-stage category as
matching criteria were performed to match the 15 patients where treatment plans
were optimized to reduce PCM dose, to the 15 patients where dose optimization of
the PCM had not been performed (Table I). For these patients the PCM was
contoured retrospectively. The Dmean
to the PCM, the superior, middle and inferior PCM substructures (PCMsup,
PCMmid and PCMinf, respectively) were extracted from the
dose volume histograms and compared. NTCP for difficulties with swallowing
solid food were estimated using a previously published model (Radiotherapy and
Oncology (2016), 118; 298-303). Mann-Whitney U-test were used to test for
differences between the groups (Optimized vs non-optimized).
Results
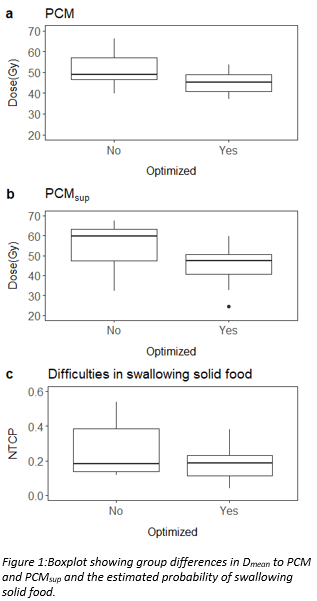
The Dmean to PCM were less than 55 Gy
in all patients in the optimized group and in 10 patients in the non-optimized
group. The Dmean was significantly higher in the non-optimized group
for the PCM (p = 0.02) and the PCMsup (p=0.03) (Figure 1a-b/ Table I).
No significant group difference was found for PCMmid and PCMinf
(Table I). Differences in estimated
NTCP was in general higher in the non-optimized group, however the difference
was not significant (p= 0.2) (Figure 1c).
Conclusion
Although the
dose to PCM was significantly reduced when applying dose constraints during the
optimization process, this was not translated into a significant reduction in
NTCP. The patient material was however limited and we recommend further
analysis in a larger patient cohort where outcome data on swallowing
dysfunctions are included.