Identifying the priority challenges of facilitating national proton beam therapy clinical trials
OC-0132
Abstract
Identifying the priority challenges of facilitating national proton beam therapy clinical trials
Authors: Lucy Davies1, Jacqui Parker1, Philip Teles Amaro1, Lee Whiteside1, Cynthia Eccles1,2, Rachael Bailey1, Sally Falk3, Julie Webb1, Louise McHugh1
1The Christie NHS Foundation Trust, Radiotherapy, Manchester, United Kingdom; 2University of Manchester, Division of Cancer Sciences, School of Medical Sciences, Faculty of Biology, Medicine and Health, Manchester, United Kingdom; 3The Christie NHS Foundation Trust, Proton Beam Therapy, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Since the UK’s first NHS high-energy proton beam therapy (PBT) centre
became operational in 2018, a significant proportion of patients referred for
treatment have been enrolled in clinical trials. External patient referrals from
healthcare organisations across the whole of the UK has highlighted a need for greater
research governance and the streamlining of complex PBT data transfer
procedures compared to existing local radiotherapy trial processes.
This work reports on the process of identifying the priority challenges
with a view to improving the proton trial pathway using an evaluative
methodology, the nominal group technique (NGT).
Material and Methods
To identify the key issues surrounding the practical implementation of PBT
clinical trials, the facilitation of patient PBT trial pathways and transfer of
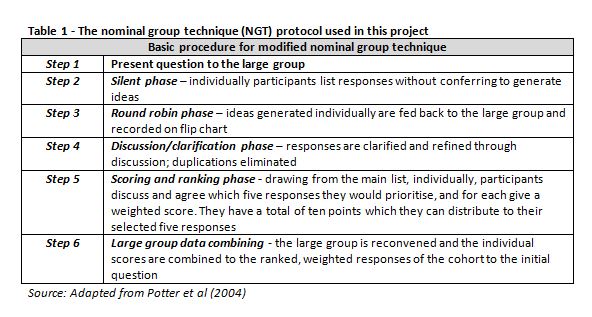
radiotherapy trial data, a modified NGT approach was used. Briefly, the
6-step modified NGT includes the presentation of a question to a group followed
by silent, round robin, discussion, scoring and data combining phases (Table 1). A panel was convened comprising
five research radiographers with experience facilitating patient pathways and reporting
radiotherapy data in adherence with PBT trials. Participants were presented
with the question: “What are the major challenges when implementing PBT
clinical trials and facilitating PBT trial-related activities?”
The results of the NGT were used to make recommendations informing local
operational policy processes, which may provide guidance for new PBT centre’s
as they become clinically operational.
Results
A total of 59 challenges were identified after combining
lists generated by each panel member. Responses were clarified, refined through
discussion and duplications were eliminated, resulting in 14 challenges
progressing to the scoring and ranking
phase. Participants individually selected 5 of the 14 challenges that they
deemed most pertinent and distributed a score (out of a possible 10 points)
across their 5 chosen challenges. Individual points were combined when the
group reconvened generating a ranked, weighted order of responses from the
cohort to the initial question. Two priority challenges scored the highest,
with every participant allocating points to these issues. These were: 1) a lack
of initial understanding of responsibilities of teams and who the relevant
stakeholders were, and 2) the nature of the national PBT service requiring the
provision of shared care across numerous multi-disciplinary teams and multiple
sites, with each organisation having their own working processes.
Conclusion
This work has identified the need
to develop shared protocols identifying and clarifying responsibilities of
multiple stakeholders to streamline PBT trial processes, promote understanding
of the respective responsibilities, and improve communication between centres referring
patients for PBT and PBT trials.
The
NGT is an effective tool for reaching consensus and identifying context-specific
priority areas for quality improvement.