Viscous Aqueous Gel Illustrating Natural Anatomy; the VAGINA method in gynaecological MRI simulation
Matthew Richardson,
Australia
PO-1871
Abstract
Viscous Aqueous Gel Illustrating Natural Anatomy; the VAGINA method in gynaecological MRI simulation
Authors: Kate Skehan1, Matthew Richardson1, Kate Martin1, Samuel Dickson2, Geetha Govindarajulu1, Swetha Sridharan1
1Calvary Mater Newcastle, Radiation Oncology, Newcastle, Australia; 2Calvary Mater Newcastle, Radiaiton Oncology, Newcastle, Australia
Show Affiliations
Hide Affiliations
Purpose or Objective
Accurate
anatomical identification is critical in gynaecological radiotherapy (RT). In our departmental
clinical practice, gynaecological patients have received two CT scans at
simulation; one full bladder scan and one empty bladder scan with tampon
in-situ. This was complimented with a full and empty bladder sagittal and axial
T2-weighted MRI scan. Diagnostic MRI exams have generated vaginal opacification
using ultrasound gel to distend and delineate the vagina due to its low viscosity
and high signal on T2 weighting. This is not recommended for gynaecological RT
planning scans, as a distended vaginal volume is not accurately reproduced at
treatment. Fusion
of planning CT and MRI scans led us to ponder if tampons do not reveal the true
shape and extent of the anatomy. We theorised a method to improve visualisation of
the true extent of the vaginal vault, without deforming the natural anatomy using
MRI simulation for RT
planning.
Material and Methods
We modified the diagnostic
opacification technique for use in MRI simulation with the alternative goal of
delineation and visualisation without distension. The standard diagnostic 60cc
of ultrasound gel, considered the correct amount for distension, was then tested
in varying lesser amounts. Aquasonic 100® ultrasound transmission gel was warmed to 36ᵒC and delivered
vaginally on the MRI couch by a Radiation Oncologist using a sterile 50ml
catheter tip syringe pre imaging. During testing both CT + tampon and MRI + vaginal
gel simulation scans were acquired for comparative qualitative imaging.
Results
After trialling
varying volumes of ultrasound gel, 10-15cc was found to be optimal for most
patients (Fig. 1).
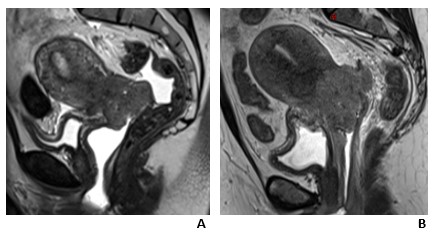
Fig. 1 Sagittal T2-weighted MRI comparing various gel volumes
showing an excessive amount of gel (A),
note deformation of natural anatomy, and optimal amount of gel (B) delineating full vaginal vault
without distension.
We observed with 10-15cc of gel the superior aspect of the vaginal vault and cervix is well visualised on T2 imaging, whilst tending not to unfold the natural fornices of the collapsed vagina (fig.2).
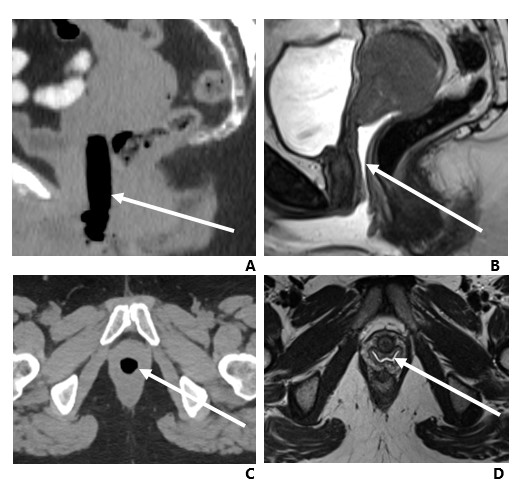
Fig. 2 A 38 year old female
with cervical squamous cell carcinoma. (A)
Sagittal CT reconstruction with tampon in-situ. (B) Sagittal T2-weighted image with vaginal gel in-situ. (C) Axial CT with tampon in-situ. (D) Axial T2-weighted image with vaginal
gel in-situ.
Conclusion
The adaption of
this diagnostic technique has facilitated more accurate contouring of the
natural vaginal anatomy in gynaecological cancers. It is also useful in
visualising disease extension into vaginal canal, which may have otherwise been
obscured by the tampon. We have ceased the second ionising CT planning scan for
gynaecological patients and removed the need for tampon insertion at the RT
simulation session. We feel this is an example of the direct clinical benefits
of increased integration of MRI simulation into routine RT clinical practice.