Estimating the dose delivered to rectum and bowel in plan of the day adaptive bladder radiotherapy
PO-1849
Abstract
Estimating the dose delivered to rectum and bowel in plan of the day adaptive bladder radiotherapy
Authors: Simon Goldsworthy1, Stuart McGrail1, Aaron Eve2, Amanda Webster3, Emma Gray4
1Somerset NHS Foundation Trust, Beacon radiotherapy, Taunton, United Kingdom; 2Somerset NHS Foundation Trust, Beacon radiotherapy physics, Taunton , United Kingdom; 3University College London Hospitals , National Radiotherapy Trials QA Group, London, United Kingdom; 4Somerset NHS Foundation Trust, Beacon radiotherapy , Taunton, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Adaptive
radiotherapy (ART) using a plan of the day (PoD) approach is a modern technique
accounting for variability in bladder volume. Inspired by participation in the
RAIDER trial (CRUK/14/016), it was deemed necessary to investigate if a simple
estimation of the delivered dose to the rectum and bowel could be calculated
based on the plans selected daily on treatment. This offers an opportunity to
learn from every patient and tailor our care plan and treatment support for
each patient when the dose to the rectum or bowel is higher, and there is a
risk of increased toxicity. The objective of this preliminary study was to develop
a simple estimation of radiation dose delivered to rectum and bowel after a
course of bladder ART.
Material and Methods
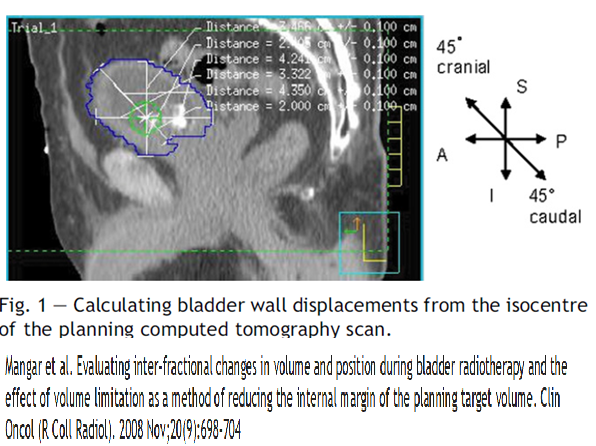
7 retrospective
patient verification CBCT data sets were evaluated. Bladder translational
displacements including a measurement in the Superior-inferior direction at 45˚were
measured (Fig 1.).
The percentage
of plans selected per treatment course, and mean D50% dose constraint for
rectum and bowel; small, medium, large plans were collated. The Common
Terminology Criteria for Adverse Events (CTAEv.4) was used to collect patient
reported acute and late (up to 24 months) rectum and bowel toxicity.
The mean
dose to rectum and bowel was calculated by multiplying the plan selected by the
mean D50%.
Example
calculation;
mean dose to D50% rectum = (small PoD% * small mean D50%) + (medium PoD% *
medium mean D50%) + (large PoD% * large mean D50%)
The estimated
mean bowel dose calculated was then validated for agreement against a composite
small bowel dose calculated in Pinnacle TPS for each patient dataset.
Results
Bladder
displacements per population (n=7) were notable in the SI and SI 45˚directions
with a systematic error of 0.98cm and 0.99cm and a random error of 0.74cm and
1.17cm respectively. The percentage of plans selected per population was 35%
small, 38% medium and 27% large. The mean dose per population was 15.94 (range
7-26) Gy for bowel and 19.98 (range 14-36) Gy for rectum. The agreement with
the TPS was 98%. The maximum CTAE for bowel and rectum acute and late
toxicities were ≤2.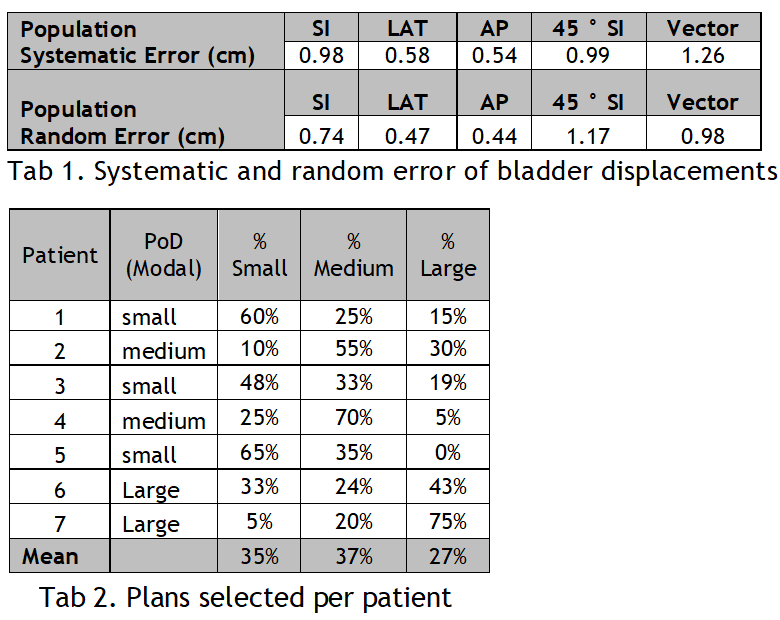
Conclusion
This
preliminary study suggests that the estimation of bowel and rectum mean D50%
dose from PoD selection can be easily calculated and validated against the TPS.
Future work should include the exploration of the relationship between the CTAE
toxifies in a larger dataset, apply this learning to other volumes or dose constraints
could be more favorable to individualising the patients care pathway.