Quantification of fat on MRI and impact on effectiveness of abdominal compression for radiotherapy
PO-1832
Abstract
Quantification of fat on MRI and impact on effectiveness of abdominal compression for radiotherapy
Authors: Mairead Daly1, Rebecca Benson2, Robert Chuter3, Abigael Clough4, Lisa McDaid4, Alan Mcwilliam1, Claire Nelder4, Eleanor Pitt4, Ganesh Radhakrishna5, Ananya Choudhury5,1, Cynthia Eccles4
1The University of Manchester, Division of Cancer Sciences, Manchester, United Kingdom; 2The Christie NHS Foundation Trust, Radiotherapy, Manchester, United Kingdom; 3The Christie NHS Foundation Trust, Medical Physics and Engineering, Manchester, United Kingdom; 4The Christie NHS Foundation Trust, Radiotherapy, Manchester, United Kingdom; 5The Christie NHS Foundation Trust, Clinical Oncology, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
High body mass index (BMI) has been identified as a
factor in reduced abdominal compression effectiveness, however, does not
consider body composition or fat distribution. Patients with higher levels of abdominal
subcutaneous adipose tissue (SAT) may have reduced effectiveness of abdominal
compression, due to attenuation of the compression force. Quantification of SAT
on cross-sectional imaging, including diagnostic MRI, is used as a biomarker in
metabolic conditions such as diabetes. This work quantified SAT percentage fat
fraction (%FF) using MRI acquired on a MR-Linac and identified the optimal
point for quantification of abdominal SAT for radiotherapy motion management.
The impact of SAT levels on reduction of respiratory motion with abdominal
compression for radiotherapy was also investigated.
Material and Methods
Eight participants (6 patients and 2 healthy volunteers)
were imaged on a 1.5T MR-Linac as part of an institutional study. T2-weighted 3D
MRI and cine-MRI were acquired with and without an abdominal compression belt. External
contour and SAT were segmented retrospectively on a single slice at three
points: the junction of vertebral levels T12/L1, L1/2, and L2/L3. The inner and
outer boundaries for SAT were defined as the external border of skeletal muscle,
and the external contour respectively. Images were segmented and evaluated by
an experienced therapeutic radiographer (RTT). %FF (SAT volume relative to
external contour volume) was calculated. Respiratory motion, defined as craniocaudal
motion of the central apex of the liver from highest to lowest point was
measured on coronal cine-MRI averaged across three breathing cycles. Bivariable
correlation analysis was used to evaluate the relationship between %FF and
change in amplitude with compression at each vertebral level, as well as the
relationship between %FF and BMI.
Results
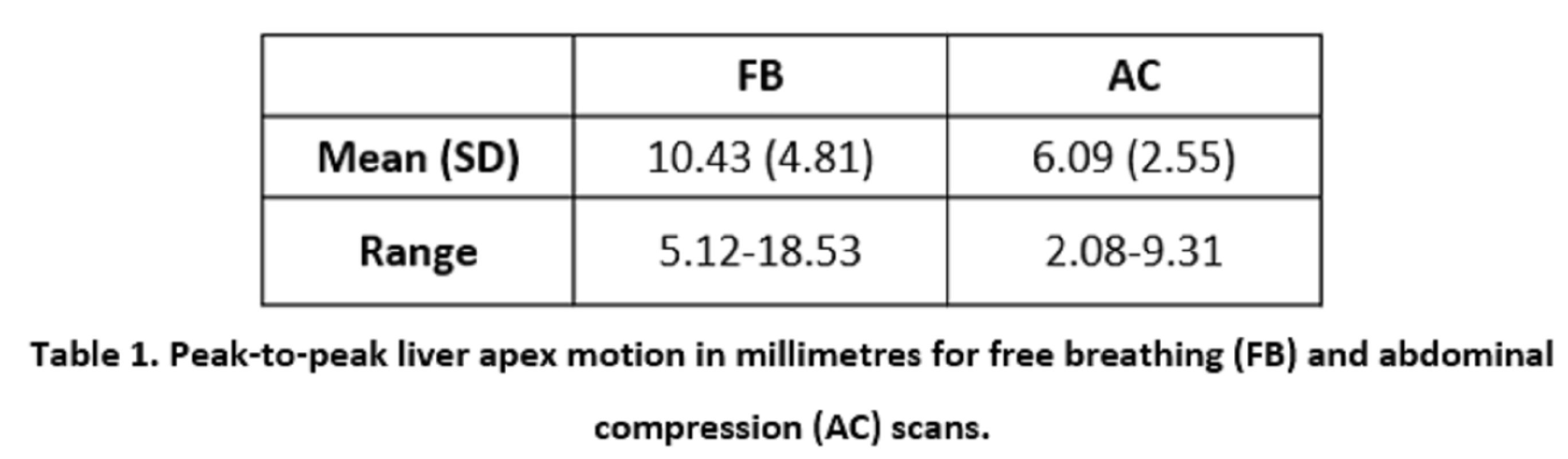
Median BMI was 27.9 (range, 25.3 – 38.0), and all
participants were considered overweight or obese. Seven out of eight
participants saw a reduction in peak-to-peak liver apex motion with abdominal
compression (Table 1). One patient volunteer saw an increase of 0.62 mm from 5.12
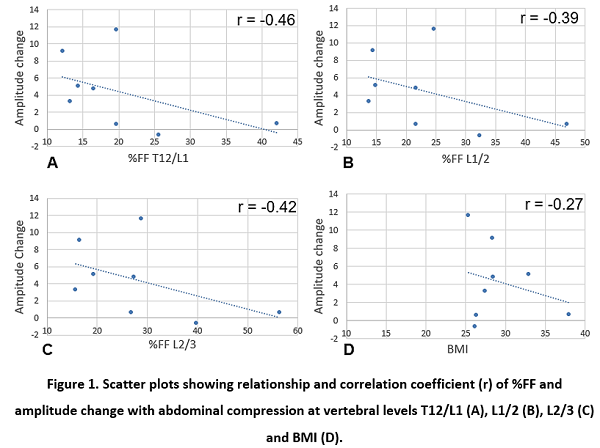
mm (BMI 26.1, %FF 41.5). Change in motion amplitude was strongly correlated
with initial motion (r = 0.85). %FF showed strongest correlation with BMI at
the level of T12/L1 (r = 0.61). %FF at T12/L1 and L2/3 had a moderate negative correlation
with amplitude change with abdominal compression (Figure 1).
Conclusion
Single-slice SAT measurements on MR images acquired on
the MR-Linac are feasible. SAT %FF demonstrated a stronger relationship with
amplitude change with abdominal compression than BMI, particularly at the level
T12/L1. In patients with smaller initial
motion (≤ 5 mm), care should be taken when using abdominal compression as
increases in liver motion are possible. This work will be validated on a larger
cohort as part of ongoing work.