IMPLEMENTATION OF INTRACAVITARY/INTERSTITIAL BRACHYTHERAPY IN THE TREATMENT OF CERVICAL CANCER
Clelia Teresa Delle Curti,
Italy
PO-1795
Abstract
IMPLEMENTATION OF INTRACAVITARY/INTERSTITIAL BRACHYTHERAPY IN THE TREATMENT OF CERVICAL CANCER
Authors: Clelia Teresa Delle Curti1, Federica Piccolo2, Brigida Pappalardi1, Rossella Margherita Mancuso3, Chiara Tenconi4, Tommaso Giandini4, Silvia Meroni5, Simona De Biaso6, Annamaria Cerrotta7
1IRCCS ISTITUTO NAZIONALE DEI TUMORI DI MILANO, Radiotherapy, Milano, Italy; 2Ospedale di Circolo e Fondazione Macchi di Varese, Radiotherapy, Varese, Italy; 3Ospedale di Busto Arsizio, Radiotherapy, Busto Arsizio, Italy; 4IRCCS-ISTITUTO NAZIONALE DEI TUMORI DI MILANO, Unit of Medical Physics, Milano, Italy; 5IRCCS-ISTITUTO NAZIONALE DEI TUMORI DI MILANO , Unit of Medical Physics, Milano, Italy; 6Università degli Studi di Milano, Unit of Medical Physics , Milano, Italy; 7IRCCS-ISTITUTO NAZIONALE DEI TUMORI DI MILANO, Radiotherapy, Milano, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
To improve target volume coverage with the
implementation of combined intracavitary and interstitial brachytherapy (ICIS-BT) in locally
advanced cervical cancer treatment.
Material and Methods
Intracavitary brachytherapy (BT) in addition
to external-beam radiotherapy (EBRT) is a standard treatment for locally advanced
cervical cancer. Interstitial BT was applied In patients with large
residual tumor volumes and minor parametrial response to improve target
coverage. In our department,
from October 2017 to November 2019, 22 patients (pts) were treated using
combined ICIS-BT for primary cervical cancer. The morphological and/or
dimensional features of the target volume (i.e. ≥30 cc) drove our choice. All pts received EBRT (VMAT) with concomitant
chemotherapy (CT) and sequential BT boost. The prescribed dose was 45Gy in 25 fractions
over 5 weeks. CT regimen was weekly Cisplatin (40 mg/m2). Image-guided adaptive
BT based on magnetic resonance imaging (MRI) was performed for all pts. According
to Gynecological GEC ESTRO recommendations, GTV, High Risk CTV (HR-CTV),
Intermediate Risk CTV (IR-CTV), bladder, rectum and sigmoid were delineated for
each BT fraction on para-axial MR images with the applicator in place.
Dose-volume histograms were calculated to evaluate doses target and organs at
risk doses (OAR). The total dose prescribed was 28Gy in 4 fractions. EBRT and
BT cumulative doses were evaluated by calculation of a biologically
equieffective dose in 2Gy per fraction (EQD2) using the linear-quadratic model with
α/β = 10Gy for tumor effects and α/β = 3Gy for late normal tissue damage. Acute genitourinary,
gastro-enteric and vaginal toxicity was monitored at each fraction and recorded
according to the CTCAE criteria version 4.03. The planning aims, according to
the EMBRACE II protocol, were achieved for all pts (i.e. HR-CTV D90 between 90 and
95Gy and GTV D98>95Gy). OAR hard constraints were never exceeded (bladder D2cm³
<80 Gy, rectum D2cm³ <65Gy, sigmoid/bowel D2cm³<70 Gy). All pts were re
optimized without interstitial needles dose contribution to demonstrate the
improvement in target dose coverage due to the interstitial component. The HR-CTV
D90 obtained with and without ICIS-BT were compared using matched pair two-tailed t-test statistics. All analyses were performed with significance level of
5%.
Results
BT
was well tolerated by all pts. Figure 1 shows the variation of CTV-HR D90 for
each patient at the first treatment fraction, with and without the contribution
of the interstitial needles. The average gain in terms of target coverage was
of 21% in favor of the ICIS-BT treatments(p value:0,0007).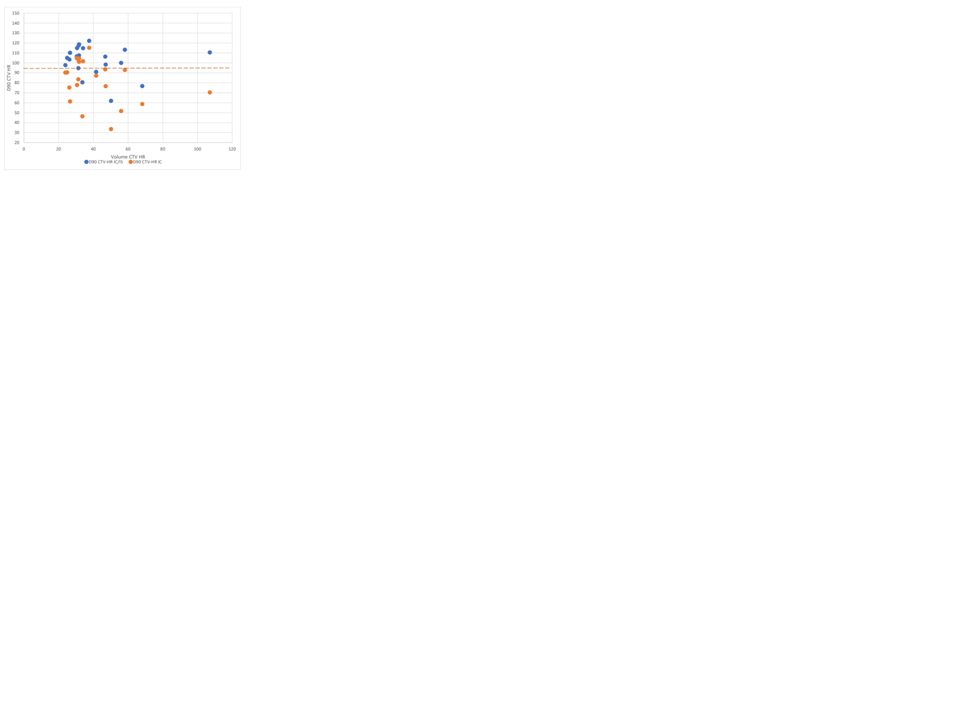
Conclusion
In pts with large tumor volumes at the time of BT, with
minor parametrial response, the concomitant implementation of the interstitial and the
intracavitary techniques allows to guarantee an adequate target coverage, with
a consequent better local control of the disease.