Evaluating diffusion weighted signal change on the MR-Linac during bladder cancer radiotherapy
Manasi Ingle,
United Kingdom
PO-1749
Abstract
Evaluating diffusion weighted signal change on the MR-Linac during bladder cancer radiotherapy
Authors: Manasi Ingle1, Matthew Blackledge2, Andreas Wetscherek3, Robert Huddart4, Susan Lalondrelle5, Shreerang Bhide5, Shaista Hafeez1
1The Institute of Cancer Research/The Royal Marsden Hospital, Radiotherapy and Imaging, London, United Kingdom; 2The Institute of Cancer Research , Radiotherapy and Imaging, London, United Kingdom; 3The Institute of Cancer Research, Radiotherapy and Imaging, London, United Kingdom; 4The Institute of Cancer Research/Royal Marsden Hospital, Radiotherapy and Imaging, London, United Kingdom; 5The Royal Marsden Hospital/The Institute of Cancer Research, Radiotherapy and Imaging, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Hybrid MRI and linear accelerator platforms such as the MR-Linac (Unity, Elekta AB, Stockholm Sweden) enable functional imaging tumour assessment during treatment. A decrease in diffusion-weighted imaging (DWI) signal and increase in apparent diffusion coefficient (ADC) is associated with complete response (CR) on diagnostic MRI. We present results of a preliminary study determining feasibility of measuring DWI signal change in bladder cancer patients treated on MR-Linac.
Material and Methods
Patients with T2a-T4, N0-N2, M0-M1 bladder cancer suitable for radiotherapy on MR-Linac were prospectively recruited to a single institutional study. Radiotherapy was delivered to the whole bladder using 30-36Gy/5-6 weekly fractions. DWI with b-values of 0, 50, 100, 250 and 1000 s/mm2 was acquired. ADC maps were created using all b-values (ADCall) and 100, 250 and 500 s/mm2 (ADCb100). Qualitative analysis of images was performed to determine best visibility of signal in tumour. DWI signal in tumour was manually contoured and mean ADCall and ADCb100 values were calculated using an in-house tool.
Results
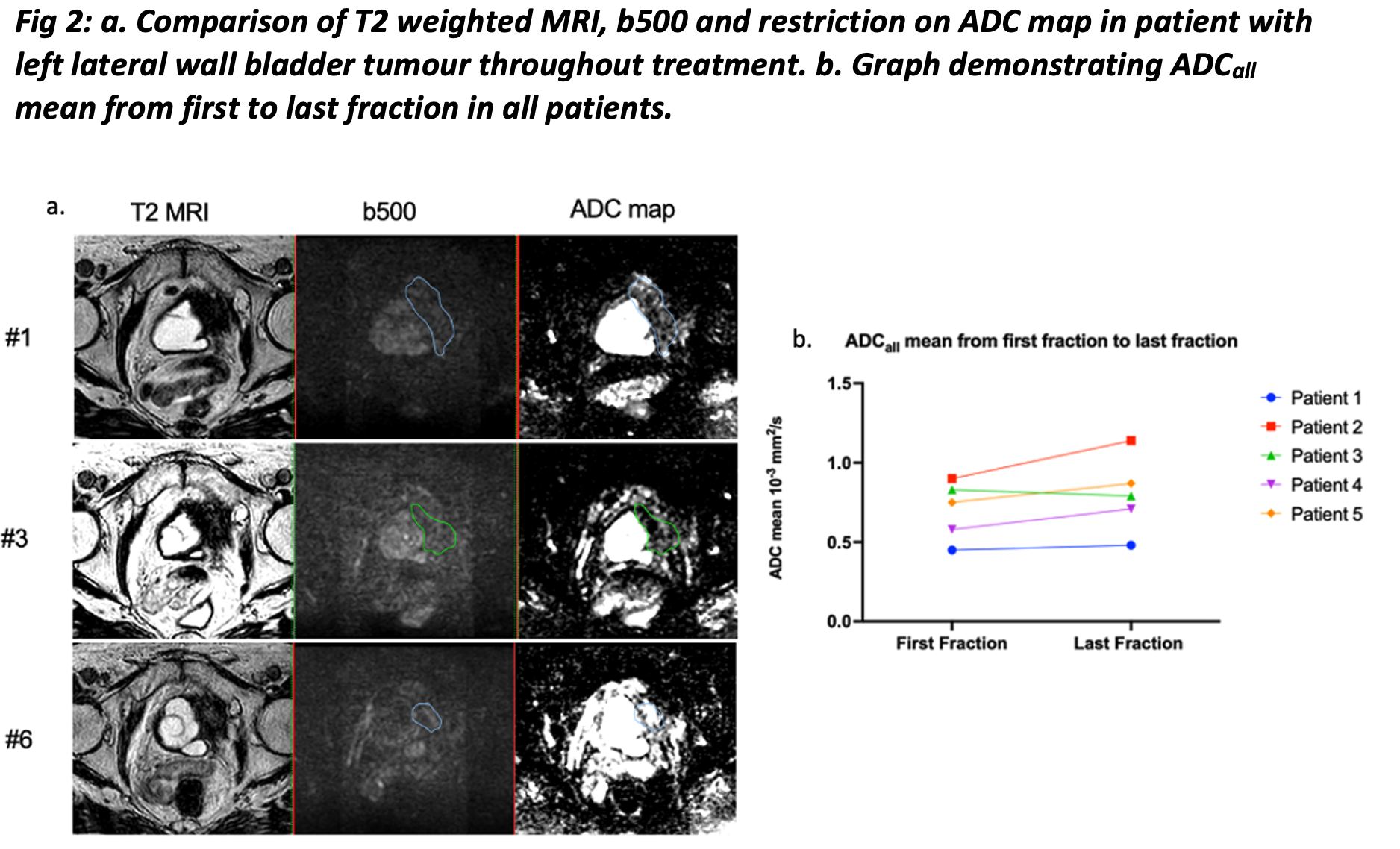
Between May 2019 and April 2021, 5 patients underwent radiotherapy on the MR-Linac for bladder cancer with DWI acquisition. Tumour signal visibility is best seen in b500 image when bladder is full (fig 1). However, during treatment when bladder is not filled tumour signal is difficult to distinguish from surrounding structures. In this situation, restriction of tumour on ADC map was better visualised (fig 2). Thus, for ADC calculation GTV is manually contoured on b500 image (GTVb500) and modified using restriction on ADC map.
4/5 patients demonstrated a non-statistically significant trend to increasing mean ADCall between first to final fraction (0.70 x 10-3 mm/s2 to 0.80 x 10-3 mm/s2; p=0.1875) (fig 2). One patient demonstrated decreasing tumour ADC mean but DWI signal in tumour was difficult to ascertain. In this patient pelvic nodal involvement was visible which demonstrated increasing ADCall mean (0.53 x 10-3 mm/s2 to 0.63 x 10-3 mm/s2) following treatment. This suggests possibility that ADC calculations are not reliable if DWI signal is not clear. All patients achieved MR assessed CR at 3-month follow-up.
ADCall mean values are 7.1- 30.5% lower than ADCb100 values. Tumour mean ADCall and ADCb100 for all patients at first fraction was 0.70 x10-3 mm2/s and 0.82 x10-3 mm2/s (p=0.0625) respectively. The difference in values is likely due to inclusion of perfusion factors present at low b-values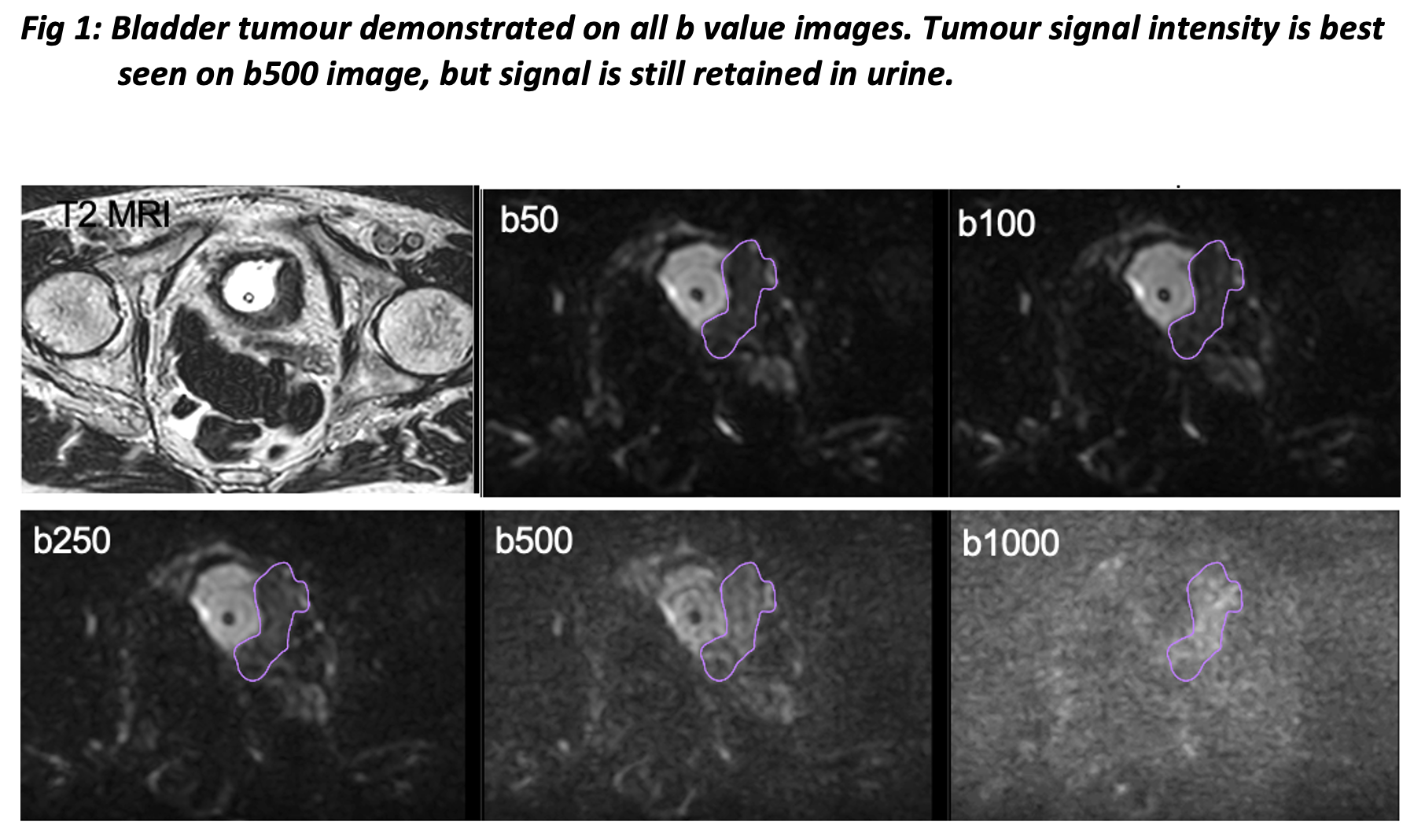
 .
.
Conclusion
Measuring ADC in bladder tumours on the MR-Linac is feasible. Difference between ADCall and ADCb100 likely reflects the intrinsic vascularity of bladder tumours and perfusion effects. Increase in ADC during treatment corresponds to CR seen on diagnostic MRI. Work is on-going to technically validate this imaging biomarker which may provide an early predictor of bladder cancer radiotherapy response.