A first-in-human prospective study on respiratory gating with mechanical ventilation for lung SABR
Loic Vander Veken,
Belgium
PO-1723
Abstract
A first-in-human prospective study on respiratory gating with mechanical ventilation for lung SABR
Authors: Loïc Vander Veken1, Geneviève Van Ooteghem2, Benoit Ghaye3, Ariane Razavi2, David Dechambre2, Antoine Delor2, Xavier Geets2
1Université Catholique de Louvain, Institut de Recherche Experimentale et Clinique (IREC), Center of Molecular Imaging, Radiotherapy and Oncology (MIRO), Brussels, Belgium; 2Cliniques Universitaires Saint-Luc, Radiation Oncology, Brussels, Belgium; 3Cliniques Universitaires Saint-Luc, Radiology, Brussels, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
Gated
irradiation during limited time windows for lung SABR allows the use of small
safety margins. This strategy therefore requires high in-treatment tumor
repositioning accuracy. This could be achieved by sophisticated on-board
imaging technology (fluoroscopy, MRI) providing real-time information on
patient’s internal anatomy. However, conventional linear accelerators are not
equipped with such devices. Moreover, patients referred for this indication often
suffer from co-morbidities that challenge the feasibility of repeated and
prolonged apneas. Mechanically-assisted and non-invasive ventilation
(MANIV) has the potential to reduce the patient's work of breathing while ensuring
excellent positional breath-holds reproducibility. We present here the first
patient successfully treated with this technique as part of a prospective trial.
Material and Methods
A 66-year-old
patient was diagnosed with stage I lung carcinoma for
whom an indication of stereotactic radiotherapy (5 x 11 Gy) was retained. A
gold fiducial was implanted in close vicinity to the tumor.
Seven days later and after one hour of coaching, the 3D planning CT was
acquired during a mechanically-induced apnea. A
back-up 4D CT was also performed. The clinical PTV was generated by a 7 mm
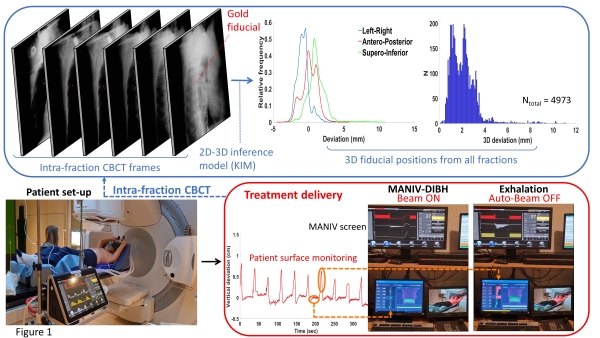
isotropic dilation of the GTV. The treatment workflow is illustrated in
Figure.1: once positioned on the couch, the patient is connected to the mechanical
ventilator which produces perpetual cycles of exhalations and 30 seconds apneas
by alternating two pressure levels with oxygen-enriched air (FiO2 =
60%). Using surface imaging, the beam was automatically interrupted when the
monitored surface was out of tolerances. The 3D residual fiducial motion during irradiation
was reconstructed off-line with a 2D-3D inference model based on intra-fraction
CBCT frames. The delivered dose to the GTV was then recomputed based on the
tumor trajectory and imaging logfiles for different PTV sizes.
Results
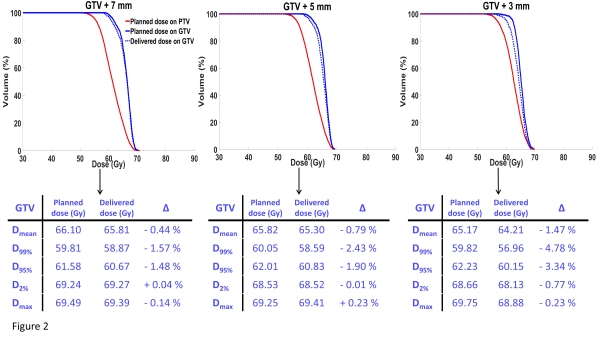
PTV
volumes generated by an isotropic GTV extension of 3 mm, 5 mm and 7 mm were 5.4
cc, 9.8 cc and 16.0 cc, respectively while PTVITV volume was 17.9 cc.
For all fractions, 98.2% of the 3D fiducials deviations during breath-holds were
below 5 mm. As shown in Figure.2, this results in high GTV dosimetric coverage
for PTV of 7 and 5 mm. The total slot time was on average 45.2 minutes [43.3 -
50.7] while the mean irradiation time was 15.6 minutes [13.5 - 19.5]. The mean
ventilation comfort score assessed on a visual analogue scale was 79.8% [70.3 -
87.9]. No abnormal vital parameters values were recorded. On average, the maximal
rise in end-tidal partial pressure of CO2 per fraction was 18.8 mmHg
[17.5-20.5].
Conclusion
Mechanical
ventilation appears to be a promising motion management technique allowing to
perform accurate, safe and well-tolerated gated stereotactic radiotherapy in
the environment of a conventional linear accelerator. More inclusions are
needed to confirm the feasibility and to recalculate dedicated safety margins
according to residual motion.