Why all left breast patients do not benefit from DIBH techniques? A retrospective analysis
PO-1701
Abstract
Why all left breast patients do not benefit from DIBH techniques? A retrospective analysis
Authors: Nagore Garcia Apellaniz1, Pedro Gallego1, Jaime Pérez-Alija1, Cristina Ansón1, Nuria Jornet1, Helena Vivancos1, Agustín Ruiz1, Marta Barceló1, Fátima Leo1, Artur Latorre1, Pablo Carrasco1
1Hospital de la Santa Creu i Sant Pau, Servicio de Radiofísica y Radioprotección, Barcelona, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Deep Inspiration Breath Hold (DIBH) is used in left-sided breast radiotherapy to reduce the dose delivered to the OARs, mainly to the heart and homolateral lung. We implemented a DIBH technique in 2016 and, since then, there has been a great effort to increase the number of patients that benefit from this procedure. Therefore, we aimed to quantify this increase and to look for improvement areas.
Material and Methods
The Varian RPM and RGSC respiratory gating systems are non-invasive devices. Our protocol considers that a patient is valid for DIBH when she achieves threshold values above 1 cm and can hold the breath around 20 seconds.
Plans were extracted from the ARIA database using the scripting API provided by Varian.
A total of 573 left-sided breast plans were retrieved, ranging from 2018 to 2021. All plans were manually reviewed and assigned to either DIBH-category or no-DIBH category.
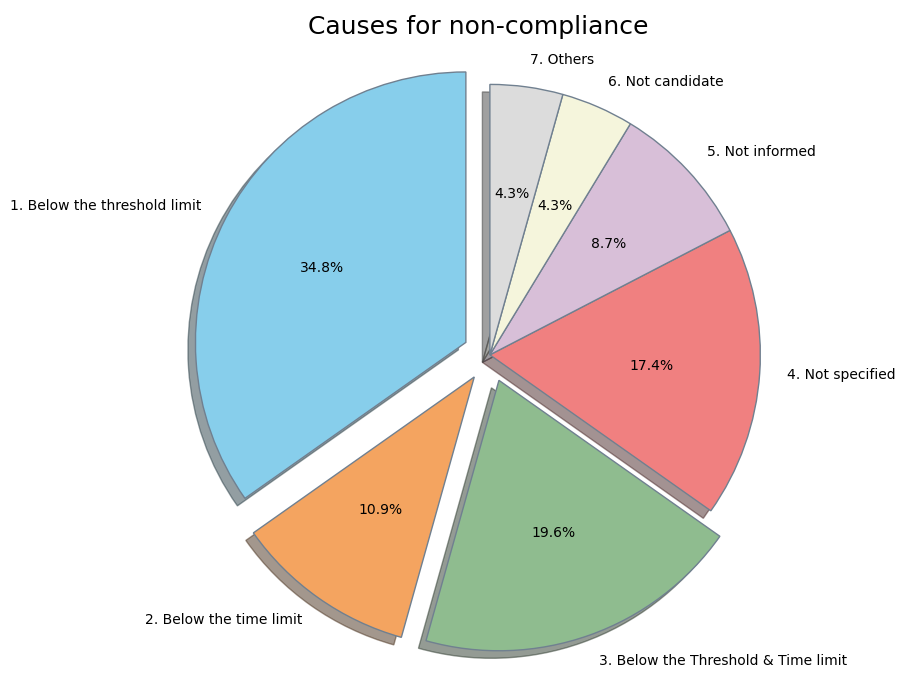
Additionally, we reviewed the CT simulation notes of the patients that did not perform DIBH in 2021. All these patients were subsequently categorized into seven categories (Figure 1). The not specified category was used for those simulations that had no reason noted down. The not candidate category was used for patients not suitable for DIBH (health issues related), while those patients who did not receive proper guidelines before the simulation and did not achieve DIBH were included in the not informed category. Finally, the others category contains causes that did not fit in the previous categories.
Results
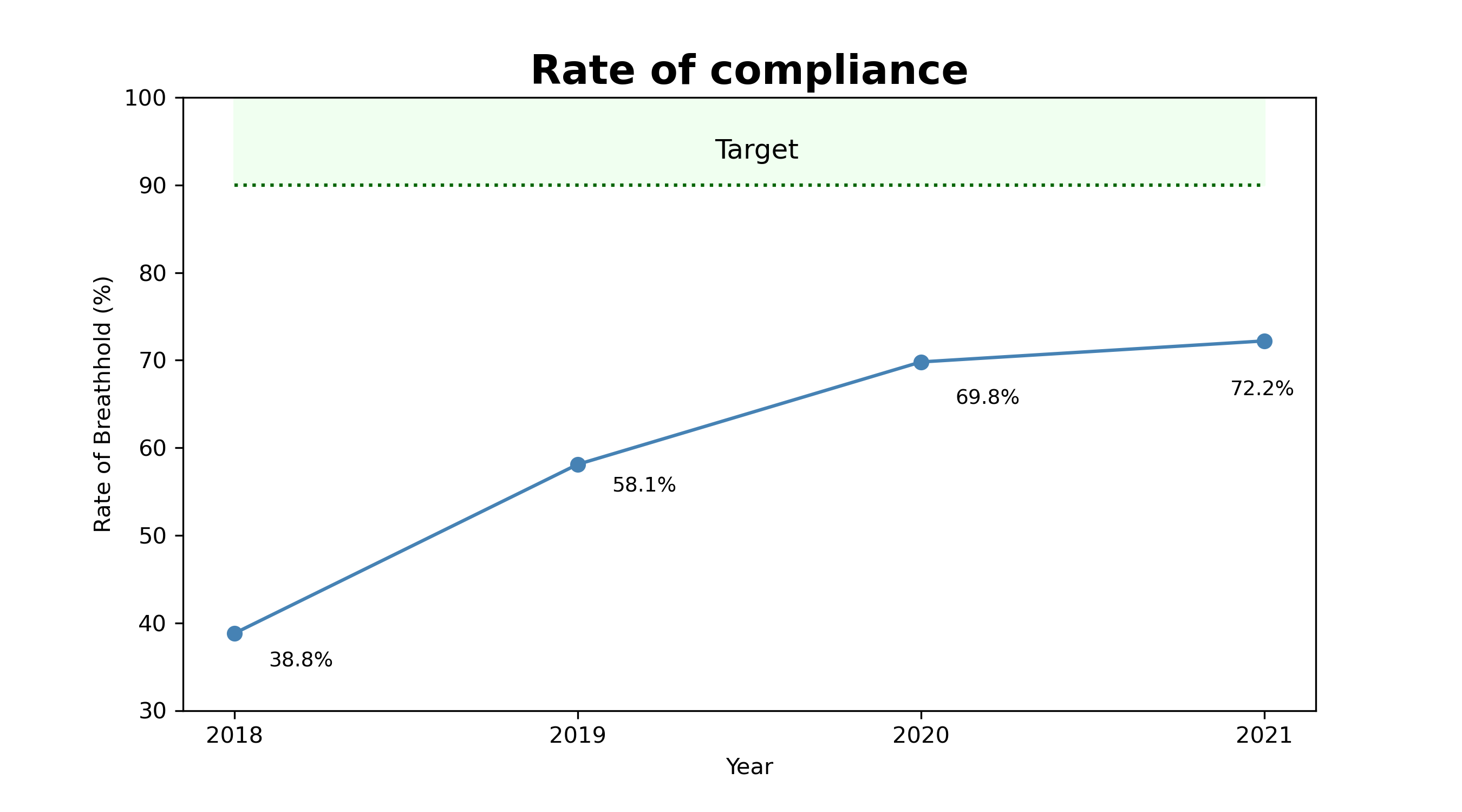
A total of 353 (61.6%) patients were able to comply with the DIBH requirements.
Figure 2 shows that since 2018, DIBH patients have increased from 38.8% to 72.2%. A total of 45 (27.8%) patients did not undergo DIBH treatment during 2021.
The not specified category shows that we have a non-negligible amount of CT simulation notes without explanation. The not candidate category is related to patients’ characteristics, so there is no room for improvement. The not informed category has been identified as the improvement area easier to work on as it can be reduced by promoting awareness of the benefits of DIBH among radiation oncologists.
Conclusion
Even though DIBH has been implemented correctly in our centre, we have reached a plateau. Published literature reports DIBH compliance rates up to 90%, showing that we still have room for improvement.
The first three categories are all related to training issues, and hence the implementation of new training programs would reduce them. Furthermore, it has been highlighted to therapists the importance of noting down the reasons (not specified category) for further analysis and improvement.
The following actions will be taken:
- Develop new training programs.
- Promote awareness of the benefits of DIBH among therapists.
- Emphasize that all CT simulation notes must be filled.