QA of dose originating from deformable image registration of planning CT to CBCT on the Ethos system
PO-1634
Abstract
QA of dose originating from deformable image registration of planning CT to CBCT on the Ethos system
Authors: Maria Sjölin1, Ivan R. Vogelius1,2, Nikolaj K. G. Jensen1, Malene E. Bak1, Flemming Kjær-Kristoffersen1, Trine J. Nøttrup1, Jeppe Friborg1, Vibeke N. Hansen1, Jens Petersen3,1
1Rigshospitalet, Department of Oncology, Copenhagen, Denmark; 2University of Copenhagen, Faculty of Health and Medical Sciences, Copenhagen, Denmark; 3University of Copenhagen, Department of Computer Science, Copenhagen, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
A deformable image registration (DIR) algorithm is part of the dose calculation chain through the Hounsfield unit (HU) assignment on the Ethos system. DIR algorithms are sensitive to individual anatomical changes and should thus be included in the patient specific quality assurance (QA) of the dose calculation. The aim of this study was to evaluate the DIR algorithm used in the ETHOS system for clinical situations where a variable amount of organ deformation can occur.
Material and Methods
We analyzed 18 adaptive treatment sessions in 8 patients treated in our clinic.
In order to estimate the dose calculation uncertainty pertaining to the DIR process of the HU, we evaluated 3 daily CT images:
- CTref: The planning CT registered to the CBCT using a 3D rigid match to determine the offset from the initial planning position.
- dpCTEthos : Ethos’ synthetic CT, based on DIR of the planning CT to the CBCT.
- dpCTPlastimatch: Independent synthetic CT generated using Plastimatch open-source software, based on DIR of planning CT to CBCT.
The two DIR methods were compared by quantifying the similarity of dpCTEthos vs dpCTPlastimatch and each of the two with the acquired CBCT data. Mean absolute error (MAE ± SD) and dice similarity coefficient (DSC) for the pelvic bones defined by HU>250 were used to measure image similarity.
The dosimetric effect of the DIR method used was investigated by recalculating the initial treatment plan on the 3 CTs. A global gamma analysis with an acceptance criterion of 3% dose difference and 3 mm distance to agreement, γ3%,3 mm ≤1, was used to evaluate agreement between the reference dose and the dose calculated with a deformed CT.
Results
Examples of the CT difference and dose gamma maps are shown in Fig 1.
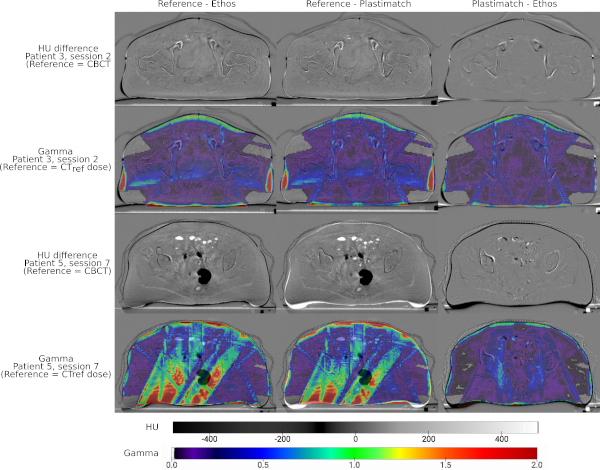
The agreement between Ethos and Plastimatch DIR was high with MAE and DSC of dpCTEthos vs dpCTPlastimatch of 33.2 ± 9.5 HU and 0.80 ± 0.07, respectively. The DSC of the Plastimatch DIR were higher than or identical to Ethos DIR in each CBCT analyzed. The MAE and DSC of CBCT vs dpCTEthos, respectively, was 53.0 ± 10.4 HU and 0.71 ± 0.06.
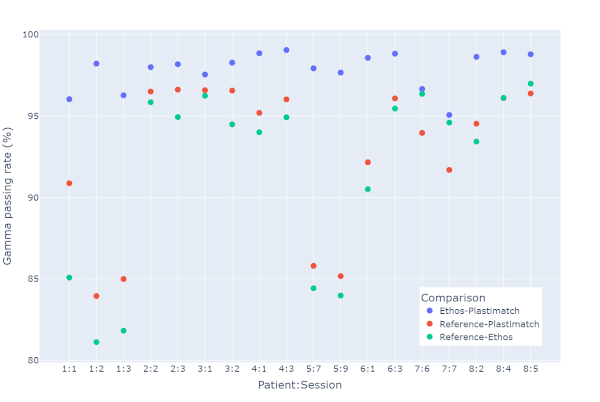
Fig.2 shows the gamma passing rates. The mean fraction of γ3%,3 mm ≤1 was 97.9 [95.1 to 99.1]% for the dose distribution on dpCTEthos compared to the dose distribution on dpCTPlastimatch confirming a good dosimetric agreement. The lowest gamma passing rate of 81.1% between the dose on the dpCTEthos and CTref. was observed for a case with a complex anatomy change with gas pockets in the planning CT perturbing the dose distribution.
Conclusion
The gamma maps indicate a small uncertainty in dose calculation introduced by the DIR algorithm implemented in Ethos and is within a clinically acceptable level. However, efforts to introduce direct HU conversion table for the CBCT are desirable.