Feasibility of acute hematologic toxicity model-based patient selection for proton beam therapy
PO-1505
Abstract
Feasibility of acute hematologic toxicity model-based patient selection for proton beam therapy
Authors: Peilin Liu1, Xi Cao1, Xian-shu Gao1, Shiyu Shang2, Jiayu Liu1, Zishen Wang3, Xuanfeng Ding4
1Peking University First Hospital, Department of Radiation Oncology, Beijing, China; 2Hebei North University, Oncology, Zhangjiakou, China; 3Hebei Yizhou Tumor Hospital, Department of Radiation Oncology, Zhuozhou, China; 4Beaumont Health, Proton Beam Therapy Center, Department of Radiation Oncology, Royal Oak,MI, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
To investigate the
potential clinical benefit of utilizing IMPT to reduce acute hematologic
toxicity for locally advanced non-small cell lung cancer (NSCLC) patients and
explore the feasibility of a model-based patient selection approach via the normal
tissue complication probability (NTCP).
Material and Methods
Twenty patients with locally advanced NSCLC
were enrolled. Volumetric modulated arc photon therapy (VMAT) and
intensity-modulated proton therapy (IMPT) plans were generated with a prescription
dose of 60 Gy in 30 fractions. A wide range of cases with varied tumor size,
location, stations of metastatic lymph nodes were selected to represent the
general cancer group. Contouring and treatment planning followed RTOG-1308
protocol. Doses to bone marrow (BM) and other organ-at-risks were compared.
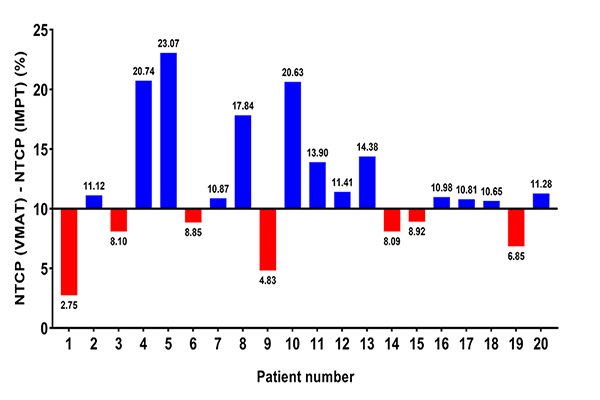
Risk of grade ≥ 3 acute hematologic toxicity (HT3+) were calculated based on
NTCP model and patients with reduction on NTCP of HT3+ (△NTCP_HT3+) ≥ 10% were
considered to 'significantly benefit from proton therapy.'
Results
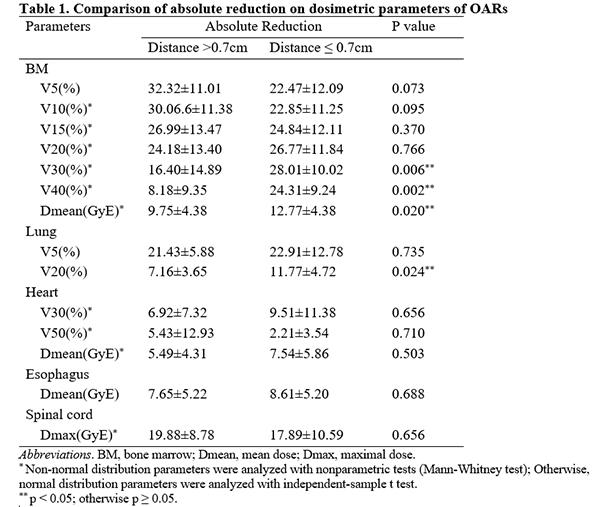
Dose to the BM, the lung,
the heart, the esophagus and the spinal cord was significantly reduced via IMPT
compared to VMAT. Tumor distance to thoracic vertebrae bodies (TVB) was
significantly associated with > 10% △NTCP_HT3+ from IMPT
to VMAT. For the patients with tumor distance ≤ 0.7 cm to TVB, the absolute
reduction of dose (mean, V30 and V40) to BM was significantly lower than that
in patients with tumor distance > 0.7 cm.
Figure.1 Possibility of HT3+ in 20 patients
Conclusion
IMPT reduced HT3+ compared
to VMAT by reducing dose to the thoracic BM in NSCLC patients. Patients with
tumor distance ≤ 0.7 cm to TVB are likely to benefit most from proton over
photon therapy