Pediatric proton whole lung irradiation
PO-1499
Abstract
Pediatric proton whole lung irradiation
Authors: Stella Flampouri1, James Janopaul-Naylor1, Roelf Slopsema1, Natia Esiashvili1, Bree Eaton1
1Emory University, Radiation Oncology, Atlanta, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
The aim of the study is to develop a treatment planning method for pediatric whole lung irradiation (WLI) with scanning proton therapy (PT) and to quantify dosimetric benefits compared to VMAT while considering the relevant proton uncertainties.
Material and Methods
21 pediatric patients with 4DCT of the entire lungs were selected for this study. Data of the patients, previously treated for a variety of indications, were acquired through a retrospective IRB. The cohort was selected to have a wide range of ages [1-18]. 12 patients were female and 8 were treated under anesthesia. The CTV covered the entire lung volume as contoured on the 4D minimum intensity projection, plus the hilum/mediastinum from 5mm above the heart to top of sternum. Prescription dose was 15 GyRBE. Treatment plans with 3 posterior fields (RPO, LPO, SPO) were robustly optimized to meet clinical goals on inhale, exhale, and under setup/range error scenarios (±5mm/±5%). Monte Carlo was used for optimization and dose calculation. A battery of interplay mitigations was used depending on the grade of diaphragmatic motion. Plan priorities were: 1. Target coverage under uncertainties and reducing dose to 2. Heart, 3. Breast tissue (f), 4. Body (integral dose), 5. Abdominal organs. VMAT plans were created with identical optimization priorities and PTV (5mm) target. Proton plan robustness evaluation was based on 28 scenarios of combined range and setup errors, 4D dose, and 4D dynamic dose calculations. VMAT plan robustness was evaluated with PTV.
Results
Proton CTV coverage was achieved for all patients on the nominal plan, error scenarios and when breathing motion was incorporated with/without interplay effects. Without compromise on robustness, the proton plans achieved increased sparing for OARs. OAR dose differences between photon and proton plans were recorded and their statistical significance was evaluated with the Wilcoxon signed rank sum test. Mean doses for the heart as a whole, cardiac substructures, breast, esophagus, liver and rest of adjacent abdomen were clinically and statistically reduced, as shown on the table.

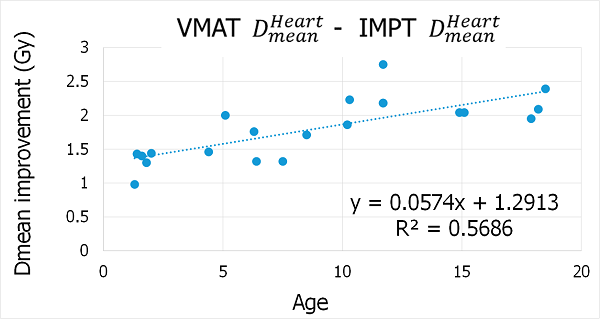
Breast (mammary glands and fatty tissue of chest wall) was the organ most spared with IMPT compared to VMAT. Statistically significant reductions of Dmax were recorded for heart, cardiac substructures and esophagus. Pearson Correlation Coefficient tests were performed to evaluate the PT dosimetric improvement as a function of patient age. There was a strong correlation for heart (whole), esophagus, breast, liver and abdomen.
Conclusion
We developed a treatment planning method for pediatric WLI to account for uncertainties including interplay effects. The proton plans provided statistically significant dose reductions compared to VMAT plans for heart, breast, esophagus and liver which may predict clinically significant reduction in late cardiac toxicity and secondary malignancies.