Image-based data mining for radiation outcomes research applies to data from children
Abigail Bryce-Atkinson,
United Kingdom
PO-1780
Abstract
Image-based data mining for radiation outcomes research applies to data from children
Authors: Lydia J Wilson1, Abigail Bryce-Atkinson2, Andrew Green2, Thomas E Merchant1, Marcel van Herk2, Eliana Vasquez Osorio2, Austin M Faught1, Marianne C Aznar2
1St. Jude Children's Research Hospital, Department of Radiation Oncology, Memphis, USA; 2University of Manchester, Division of Cancer Sciences, Faculty of Biology, Medicine and Health, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy
research increasingly focuses on managing long-term morbidity and mortality of
curative treatments. Such research relies on knowledge of the relation between
radiation exposures and their biologic effects. Critically, this relation is
often uncertain or unknown. Image-based data mining (IBDM) is a voxel-based method
for analyzing dose response that has shown promise in studies of adults with
cancer. Age-related anatomic variations, however, complicate its applicability to
children. We recently successfully applied IBDM to children with simplified
simulated radiation treatments. In this study, we tested its efficacy using simulated
but clinically realistic dose distributions.
Material and Methods
We
used CT images from 167 children (age 10 months to 20 y) who previously
received radiotherapy for primary brain tumors. We randomly divided the cohort
into simulated “effect” and “no effect” groups and modified their clinical dose
distributions by introducing a systematic dose discrepancy between the
brainstems of patients in each group. The IBDM method comprises two steps:
deformable image registration (DIR) to a reference anatomy and voxelated dose
comparison. Based on previous results, we selected the CT dataset from the patient
with the median brain volume as the reference anatomy. We quantified the
accuracy of DIR via contour-distance and center-of-mass analyses in 5 routinely
delineated brain structures. Dose comparisons comprised permutation tests with
1000 permutations. We quantified the voxel-wise accuracy with sensitivity,
positive predictive value (PPV), and dice similarity coefficient (DSC) comparing
the reference brainstem to the volume in which IBDM identified a dose
discrepancy. We performed these tests at three simulated “effect” rates, a baseline
of 50% and two rates representative of common side effects of cranial
irradiation in children: 20% and 10%.
Results
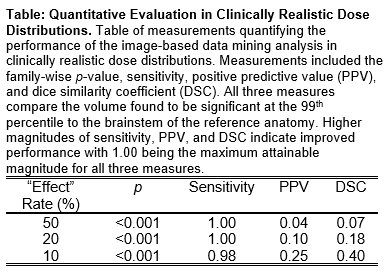
DIR
accuracy was < 2 mm (average contour distance) and < 3 mm (center of mass).
Permutation tests correctly identified the difference between dose
distributions of the “effect” and “no effect” groups (p < 0.01) at all three
simulated effect rates (Table). IBDM consistently recognized the dose differences in
the brainstem with a minimum sensitivity of 0.98, but over-estimated the
sensitive region, likely because of implicit correlations in the dose
distributions (Table, Figure). PPV and DSC improved with decreasing effect rate as the
overestimate of the sensitive region was reduced, reaching maxima of 0.25 and
0.4, respectively, at the 10% simulated effect rate (Table, Figure)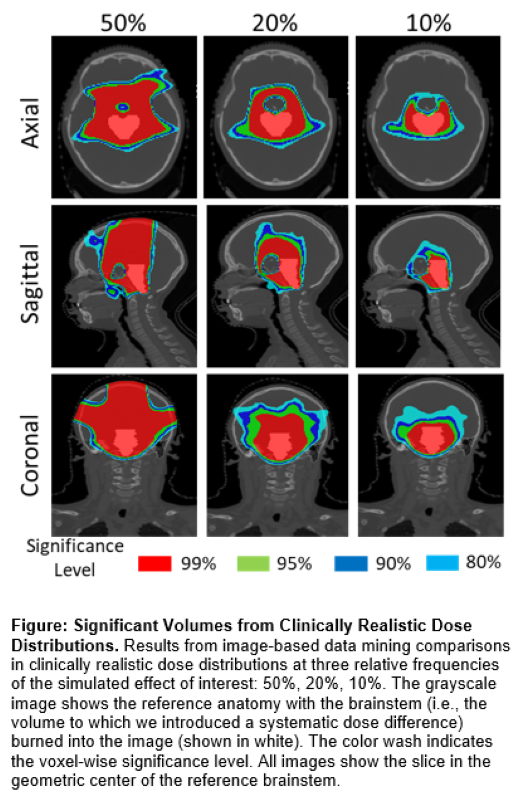
 .
.
Conclusion
This
work shows it is feasible to perform IBDM for pediatric data despite large
anatomic variations among patients. This approach enables an unbiased
exploration of the spatial dose-effect relation in children. A deeper understanding
of this relation can inform treatment planning and survivorship care to avoid
treatment-related morbidity and mortality and improve long-term quality of life
of childhood cancer survivors.