Pain as the evaluation criterion for bone metastasis radiosensitivity.
Natalya Bychkova,
Russian Federation
PO-1471
Abstract
Pain as the evaluation criterion for bone metastasis radiosensitivity.
Authors: Natalya Bychkova1, Evgeny Khmelevsky1
1P.A. Hertsen Moscow Oncology Research Institute – Branch of the National Medical Research Radiological Centre Ministry of Health of Russia, Radiotherapy Department, Moscow, Russian Federation
Show Affiliations
Hide Affiliations
Purpose or Objective
The search
for evaluation criterion for the radiosensitivity of metastases in the skeleton
and the assessment of the comparative radiosensitivity of bone metastases of
various origins.
Material and Methods
To
identify the relationship between pain and other clinical symptoms, 810 cases
of bone metastases with persistent pain syndrome were analyzed. 3D-conformal or IMRT / VIMAT radiotherapy was
performed for bone metastases of various origins and localization. Radiotherapy
protocol included hypofractionation regimes of 2, 3 or 4 fractions of 6,5 Gy
with total dose of 13-26 Gy. The effectiveness of
radiotherapy was assessed by the frequency of complete and partial pain relief,
the degree of pain regression relative to baseline, the risk and timing of pain
relapse.
Results
The
severity of pain directly correlated with gender, lesion length and little associated
with pathological fracture. The intensity of pain did
not depend on the primary tumor and bone metastases localization and did not
correlate with the presence of neurological deficit. The overall
effectiveness (сomplete and partial pain relief) of radiotherapy was 96.2%, complete
response rate (CRR) – 56.2%, partial response rate – 40.0%. Pain relapse rate
was 8.6%, on average after 9.5 months after irradiation. The independent
predictors of the CRR were: the initial pain intensity [hazard ratio (RR):
0.48, confidence interval (CI): 0.40-0.58; p = 0.0001], dose/number of
fractions (RR: 1.26, CI: 1.07-1.50; p = 0.0059) and primary tumor site (RR:
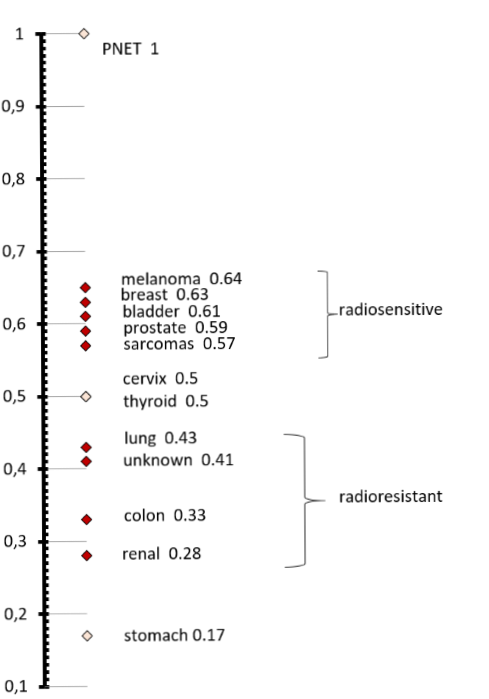
0.95, CI: 0.92-0,99; p = 0.0053). We constructed a scale of comparative
radiosensitivity of bone metastases of various primary tumors, taking into
account the complete response rate and the probability of surviving without
pain relapse for 6, 12 and 24 months after radiotherapy. The radiosensitive
group included metastases from breast and prostate cancer, melanoma, bladder
and PNET (CRR 60% or more), the radioresistant group - metastases from unknown
origin, colon, stomach and kidney cancer (CRR 40% or less). The scale of radiosensitivity is shown in Image.
Conclusion
Complete
pain relief turned out to be the most significant clinical criterion for
assessing the effectiveness of radiation therapy of bone metastases. Completeness
and persistence of the analgesic effect may reflect the real radiosensitivity
of bone metastases. More than 95% overall effectiveness of radiotherapy for
bone metastases, with pain relapse rate of less than 10% of cases, allows us to
consider irradiation in doses of 19.5-26 Gy, in 3-4 fractions of 6.5 Gy, the
preferred treatment for multifocal lesions. Dose escalation in patients with
bone metastases of kidney, colon, lung cancer and metastases from unknown
origin seems to be justified in the cases with a life expectancy of more than a
year.