Cost-Effectiveness аnalysis of radiation therapy techniques for bone metastases
Yevgeniy Ishkinin,
Kazakhstan
PO-1470
Abstract
Cost-Effectiveness аnalysis of radiation therapy techniques for bone metastases
Authors: Yevgeniy Ishkinin1, Ruslan Ibrayev1, Rauan Raimbekov1, Kuanish Rayimzhanov1, Tatyana Antropova1, Kair Datbayev1, Radmila Akhunova1
1Almaty Oncology Center, Radiation Oncology, Almaty, Kazakhstan
Show Affiliations
Hide Affiliations
Purpose or Objective
Assessment of clinical and economic efficiency
of 3DCRT and IMRT techniques for palliative radiotherapy (RT) of patients with symptomatic bone metastasis.assessment of clinical and economic efficiency
of 3DCRT and IMRT techniques for palliative radiotherapy (RT) of patients with symptomatic bone metastasis.
Material and Methods
A retrospective cost – effectiveness analysis of
143 patients received palliative RT 4 Gy to 20 Gy on symptomatic bone
metastasis on TrueBeam STx. Median
follow – up was 10.5 month. Compliance with the ethical principles 83
(58%) 3DCRT patients, 60 (42%) IMRT patients. The criterion for the choice of
the irradiation technique, was a discussion with an evaluation of treatment
plans for the dose to critical organs and a comparison of all pros and cons. IGRT by CBCT was used in every
fraction and did not take into account the direct cost. Incremental cost-effectiveness ratio - quality adjusted life-year (QALY) per direct costs. QALY - multiplication
of median survival time in year and quality of life index (QoL index) calculated according to the ratio of pain
relief to the degree of radiation complications. Assessment of pain relief
using a 10-point Brief Pain Inventory (BPI) scale, the difference in scores
before the onset of RT and 1 month after the end of RT. Radiation reactions
were assessed using a four degree RTOG scale 1 month after the end of RT. Survival curves were constructed according of
Kaplan and Meier method. Comparison of survival curves using Log
rank test by Pearson chi – square (χ2) using IBM software SPSS statistics
version 23.0.
Results
For IMRT patients
mean BPI scores were 7.6 before RT, and 2.3 after RT; pain relief by 5.3 points
was estimated. For 3DCRT patients mean BPI scores
were 7.1 before RT, and 2.5 after RT; pain relief by 4.6 points was estimated. Radiation reactions by
RTOG scale was 1.17 and 1.52 for IMRT and
3DCRT techniques respectively. Mean direct costs was 288.7 and 145.2 Euro per patient for IMRT and 3DCRT techniques
respectively. Mean QoL index was 4.88 (n=
60, SD =1.55) and 3.40 (n= 83, SD =1.41) for IMRT and 3DCRT respectively. IMRT technique showed significantly better
survival results overall survival 70.0% compared to 3DCRT overall survival 51.8%, differences are
statistically significant χ2 = 5.36, df = 1, p = 0.021 (Figure 1).
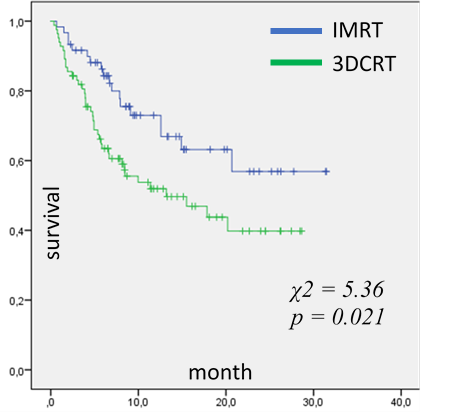
Figure 1 – Techniques survival
curves by the method of Kaplan and Meier
For IMRT patients, the median survival time was
21.9 months, SE 1.8 months, 95% CI (18.4 - 25.5), For 3DCRT patients, the
median survival time was 15.6 months, SE 1.4 months, 95% CI (12.9 - 18.4). Quality-adjusted
survival was 1.8 and 1.3 years for IMRT and 3DCRT respectively. Quality-adjusted life year (QALY) 0.89 gained for IMRT and 0.44 for and 3DCRT respectively. Per 1 QALY
was 324.1 euro for IMRT and 328.5 euro for 3DCRT techniques. This resulted in an incremental cost-effectiveness ratio 3.2 euro
Conclusion
IMRT was cost-effective beneficial compared to 3DCRT in the palliative treatment of
symptomatic bone metastasis.