The impact of post-operative radiotherapy (PORT) in patients with thymomas and thymic carcinomas
PO-1458
Abstract
The impact of post-operative radiotherapy (PORT) in patients with thymomas and thymic carcinomas
Authors: Gianluca Vullo1, Giuseppe Facondo1, Riccardo Carlo Sigillo1, Alfredo Priore1, Margherita Rotondi2, Maurizio Valeriani3, Vitaliana De Sanctis1, Mattia Falchetto Osti1
1UO Radioterapia Oncologica, Sapienza Università di Roma, AOU Sant'Andrea Roma, Radiation Oncology, Rome, Italy; 2UO Radioterapia Oncologica, Sapienza Università di Roma, AOU Sant'Andrea Roma , Radiation Oncology, Rome, Italy; 3UO Radioterapia Oncologica, Sapienza Università di Roma, AOU Sant'Andrea Roma, Radiation Oncology, Rome, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
The role of postoperative adjuvant radiation therapy (PORT)
remains controversial. The purpose of this study was to evaluate outcomes and
toxicities of PORT in a series of patients with thymoma or thymic carcinoma.
Material and Methods
We
retrospectively analysed 27 consecutive patients (17 thymomas, 8 thymic carcinomas)
who underwent surgery with a curative intent and PORT to the mediastinal
surgical bed and microscopic/macroscopic disease, if present, from 2006 to 2020
at our institution. Eight patients received neo-adjuvant chemotherapy prior to
surgery. Surgical margins status was
reported as follow: R0
resection (microscopic negative margin) was achieved in 14 patients, R1 (microscopic
positive margin) in 11
patients and R2 (macroscopic positive margin) in 2 patients. According
to Masaoka-Koga staging system 4, 6, 13 and 4 patients were stage I, II, III
and IV of disease, respectively. Acute
toxicities were graded according to the RTOG/EORTC scoring system and late
toxicities where scored according to the SOMA (symptoms, objective, management,
analytic) scoring system. The Kaplan Meier method was used to assess overall
survival (OS), relapse-free survival (RFS) and metastases-free survival (MFS). Sub-group
analysis was performed stratifying patients with R0 vs R1-2 resection margins, patients
staged I-II vs III-IV stages and patients with A-AB-B1 vs B2-B3-0 histologies.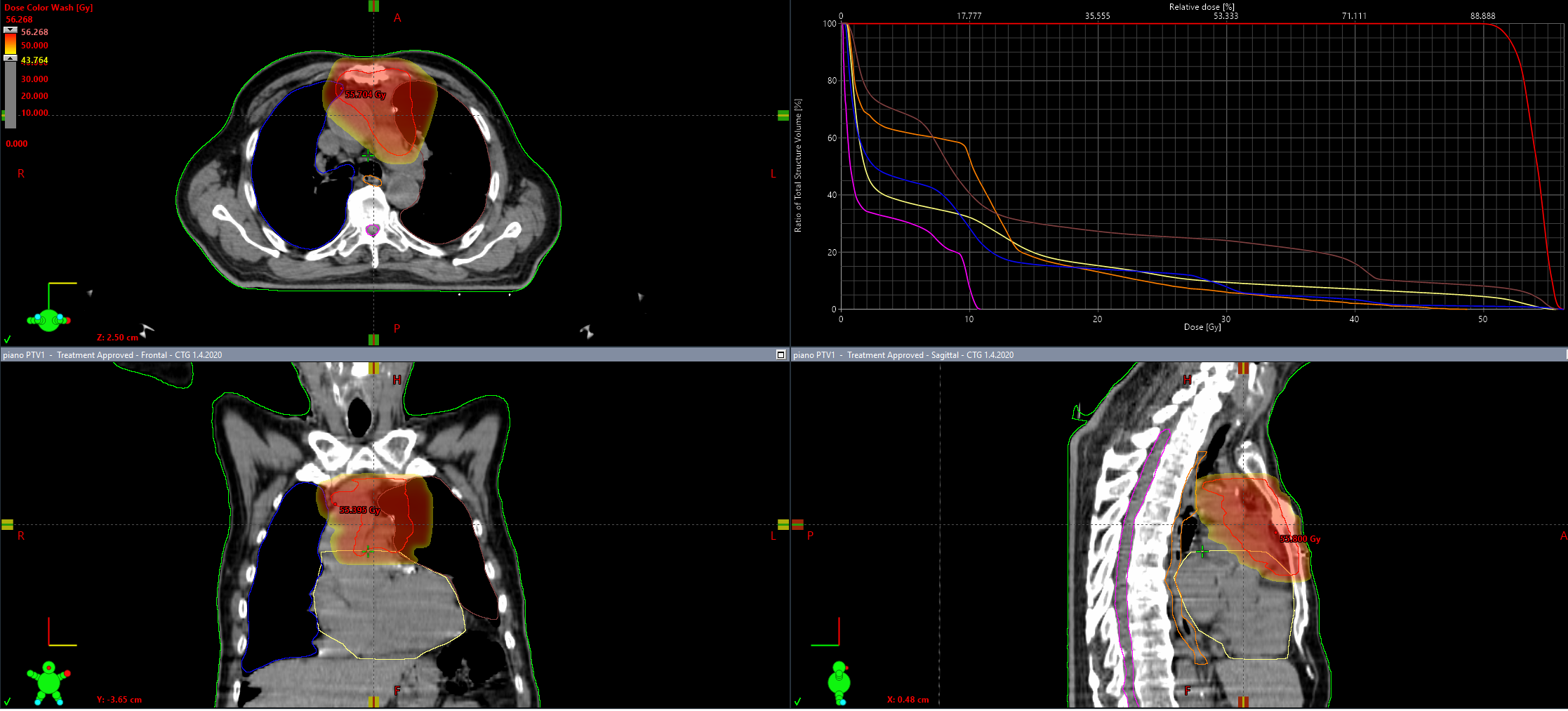
Results
PORT
was administered with 3-dimesional conformal radiotherapy in 23 patients while 4
patients were treated with intensity-modulated radiotherapy. The median planning target volume (PTV) was 250cc
(range 60-610). Median dose was 54 Gy delivered using conventional
fractionation (2 Gy daily). Median follow-up was 54 months. OS at 1- and 5-years
was 96.3% and 89%. One- and 5-year RFS was 100% and 83%. MFS at 1- and 5-years
was 92% and 67%. Patients with stages III-IV had worst 5-yers OS and MFS
compared to stages III-IV, 83 vs 100% (CI 95%: 1.16-2.06; p 0.03)
and 45 vs 100% (CI 95%:
1.42-2.8; p 0.01). WHO histologies B2-B3-0 showed
worst 5-years OS and MFS compared to A-AB-B1 group, 82.6 vs 100% (CI 95%: 1.27-2.2; p 0.02) and 46.6 vs
100% (CI 95%: 1.2-2.6; p 0.02) . No acute nor late G3-4
toxicities were observed.
Conclusion
PORT
in patients with thymic malignancies
achieved good local control and a safe toxicity profile.
Patients with III and IV Masaoka stage and WHO B2-B3-0
histology had significant worst OS and MFS.