Eight patients (57%) reached mPR, being fully
complete in 4 of them. On univariate analysis, mPR rates were higher for female
patients, older patients, thigh location, smaller tumor size (<14cm), low
grade tumors and liposarcoma histology although these differences were not
statistically significant, probably due to low number of analyzed patients.
However, addition of preoperative chemotherapy to radiation treatment associated
higher probability of mPR. Complete analysis of relationship between mPR and
clinical and epidemiological variables is detailed in table 2.
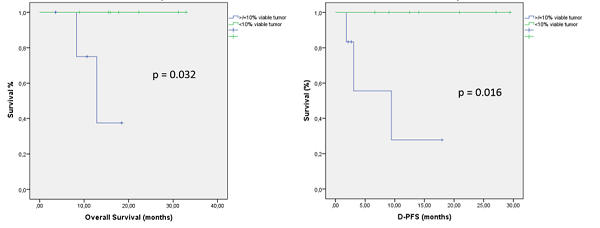
With a median follow-up of 13 months (7 – 19), 12
patients are alive, 2 patients died from distant tumor progression and no
patient suffered from local relapse. Median overall survival (OS), local
progression free survival (L-PFS) and distant progression free survival (D-PFS)
times are not achieved. Actuarial 2-year OS and D-PFS are 79.5%, and 72.4%
respectively.
mPR is related to a statistically significant
better OS (p=0.032) and better D-PFS (p=0.016). The absence of mPR was
associated with higher risk of developing distant metastases (100% vs 36.4%, p
= 0.051).
Treatment
tolerance: 5 patients (35.7%) presented grade 1-2 acute skin toxicity after
radiation treatment. Post-surgical complications: 5 patients (35.7%) had
post-surgical seroma, 1 patient (7.1%) had neuropathic pain and 8 patients
(57.1%) had wound complications. Five patients did not experience any degree of
radiation or postsurgical side effects.