CT images
were taken using a Toshiba Aquilion CT scanner at 120 kV, while CBCT images were
collected using the on-board XVI system on an Elekta Synergy linear accelerator
with a fast head and neck scanning protocol (200° rotation,
100 kV, small FOV and no filter).
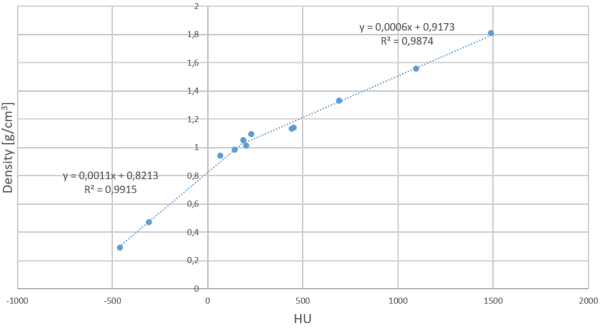
First, a
site-specific conversion (SSC) curve for HNC was created by placing Gammex
phantom inserts with known mass densities into a small custom-made phantom
(14x14x11 cm³), resulting in a bi-linear SSC curve for HNC (figure).
Secondly, a
patient-specific conversion (PSC) method available in RayStation TPS was used,
automatically attributing different ranges of HU values to 6 materials (air,
lung, adipose tissue, cartilage/bone and other high-density material) with
corresponding mass densities.
The SSC and
PSC methods were evaluated on the anthropomorphic Alderson RANDO phantom as
well as on 7 patient data sets. Only HNC patients with a re-planning CT (rCT)
for treatment adaptation were retrospectively selected. Dose calculation was
performed on the first re-planning CBCT (rCBCT). All patients received VMAT with 6MV photons
and a SIB up to 69.12 Gy in 32 fractions. Dose calculations were performed in
RayStation v9 using the CC algorithm.
Dose
comparisons between rCT, SSC-rCBCT and PSC-rCBCT were performed by means of
DVHs, dose statistics and 3-D gamma (3%, 3mm) maps. PTV and OAR ROIs were delineated
on rCT and transferred onto the rCBCT using a rigid registration between both
image sets.
To evaluate
the potential aid of both methods in clinical decision making, the clinical
goals of the original treatment plan were evaluated on the CBCT’ images on
which the decision to re-plan was based.