Inter-fraction error analyses and rectal and bladder volume variations using CBCT in prostate cancer
PO-1415
Abstract
Inter-fraction error analyses and rectal and bladder volume variations using CBCT in prostate cancer
Authors: Consuelo Rosa1,2, Marzia Borgia1, Marco Lucarelli1, David Fasciolo1, Annamaria Vinciguerra1, Antonietta Augurio1, Stefano Marcucci1, Luciana Caravatta1, Michele Marchioni3, Marta Di Nicola3, Domenico Genovesi1,2
1SS. Annunziata Hospital, Department of Radiation Oncology, Chieti, Italy; 2G. D’Annunzio University, Department of Neuroscience, Imaging and Clinical Sciences, Chieti, Italy; 3G. D'Annunzio University, Laboratory of Biostatistics, Department of Medical, Oral and Biotechnological Sciences, Chieti, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Purpose: In prostate cancer (PC) patients set-up errors can vary the prostate position between a planned Computed Tomography (CT) and Cone Beam CTs (CBCT) performed during radiotherapy (RT). Furthermore, pelvic organ motions with bladder and rectum filling variations could emphasize the variation in position of the prostate. Our aim is the evaluation of inter-fraction prostate motion, in empty rectum and controlled bladder filling, on planned-CT and CBCT.
Material and Methods
Material and Methods: We retrospectively evaluated thirty-three PC patients analyzing the first daily CBCTs performed in the first four days of RT, calculating the average shifts in all the three axes (x, y and z) and then repeating CBCT once a week after the correction of these prostate shifts. For each patient, we evalued rectum and bladder volumes on each planned-CT and CBCT. We calculated the median shift variations on all three axes and rectum and bladder filling variations between planned-CT and CBCTs on the first four CBCTs, on the following weekly CBCTs and for the total of CBCTs. Linear regression mixed models taking into account the random effect of repeated measures were employed, to identify correlation between median prostate shifts and rectum and bladder filling variations.
Results
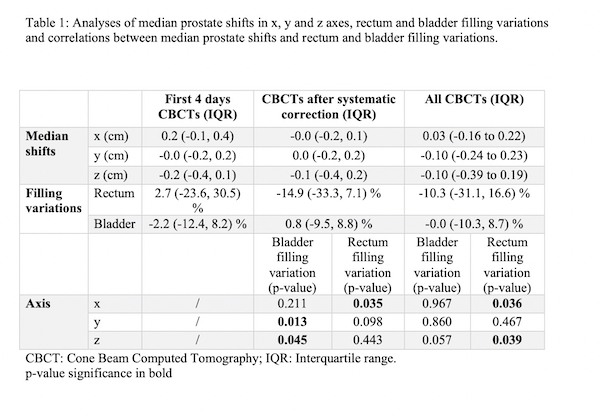
Results: We examined a total of 443 CBCTs. Table 1 reported results of median shifts and rectum and bladder filling variations calculated for the first 4 CBCTs, for the following weekly CBCTs and for the total of CBCTs. For all CBCTs median prostate displacements along the three axes (x, y and z) averaged over all patients were: 0.03 (IQR: -0.16 to 0.22) cm in x, -0.10 (IQR: -0.24 to 0.23) cm in y and -0.10 (IQR: -0.39 to 0.19) cm in z, and median rectum and bladder filling variation were -0.0 cc (-10.3, 8.7) and -27.3 cc (-109.5, 44.7), respectively. Performing the analyses of all CBCTs for relationship between prostate shift along all three axes and rectum and bladder filling variations, a statistically significant correlation was demonstrated only for rectum only in x and z axes (p=0.036 and p=0.039, respectively). Moreover, correlations analyses in CBCTs obtained after systematic set up correction found a statistically significant in y and z axes (p=0.013 and p=0.045, respectively) for bladder and in x (p=0.035) for rectum filling variations.
Conclusion
Conclusion: Daily treatment uncertainties related to setup and organ motion seems to be well controlled with the use of Image Guided Radiotherapy (IGRT). Our results seem to validate our setup protocol for rectum and bladder preparations demonstrated by small prostate shifts.