Two hundred and
four patients were included. Median age at diagnosis was 79.0 years [55.0 –
94.0] and median follow-up was 41.3 months [1.0 – 243.5]. Local and metastatic recurrences occurred in 29 patients (17%) and 60 patients (36%), respectively.
The 4-year OS and PFS rates were 46% [37.5% – 54.4%] and 28.9%
[21.7% – 36.5%], respectively. There was significantly more hydronephrosis in the high NLR
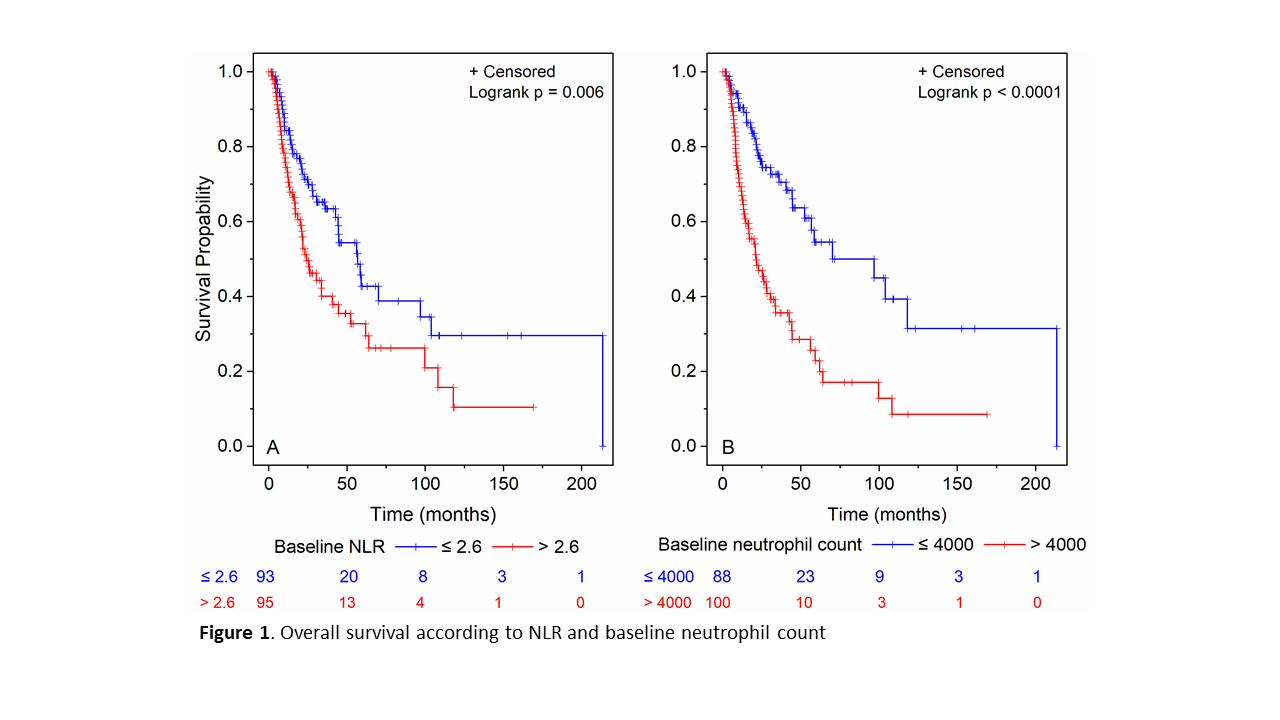
(>2.6) group (41% vs 24%, p=0.02). Median OS was significantly lower in
patients with NLR>2.6 compared to patients with NLR≤2.6 (24.1 months [18.6 – 40.6] vs 56.8 months [42.7 – 96.8], p=0.006) (Fig 1). Median OS was significantly lower in patients with PNN > 4000/mm3 compared to patients
with PNN≤4000/mm3(24.1 months [14.1 – 30.5] vs 70.1 months [52.4 –],
p<0.001). By univariate analysis, T3-T4
stage (HR=1.97, 95%CI [1.22–3.17]; p=0.005), hydronephrosis (HR=1.69, 95%CI
[1.11 – 2.58], p=0.02), PNN >4000/mm3 (HR=2.74,
95%CI [1.77 – 4.24], p<0.001), and NLR>2.6 (HR=1.77, 95%CI
[1.17 – 2.67], p=0.007) were significantly associated with shorter OS. By
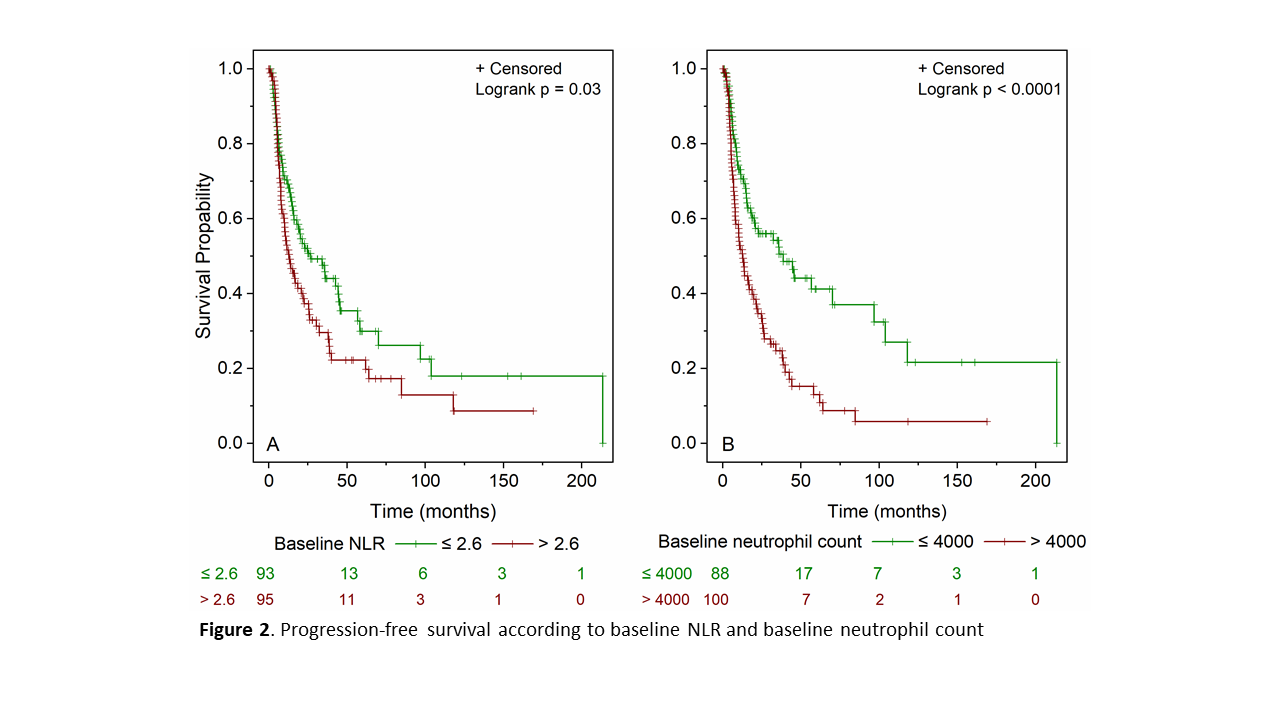
multivariate analysis, only PNN>4000/mm3 was significantly associated with shorter OS (HR=2.95, 95%CI [1.67 – 5.21], p<0.001). Median PFS was significantly
lower in patients with NLR>2.6 compared to patients with NLR<2.6 (13.1 months [9.6 – 21.8] vs 26.7 months [15.9 – 44.7], p=0.03) (Fig 2). Median PFS was significantly lower in patients with PNN > 4000/mm3 compared to patients
with PNN ≤ 4000 (12.7 months [8.0 – 19.0] vs 38.8 months [18.6 – 96.8],
p<0.001). By univariate analysis, T3-T4
stage (HR=1.95, 95%CI [1.27 – 3.01], p=0.002), hydronephrosis (HR=1.83, 95%CI
[1.27 – 2.65], p=0.001), PNN >4000/mm3 (HR=2.10,
95%CI [1.45 – 3.04], p<0.001) and NLR >2.6 (HR=1.49, 95%CI [1.04
– 2.13], p=0.03) were significantly associated with shorter PFS. By
multivariate analysis, only PNN>4000/ mm3 was significantly associated with shorter PFS (HR=1.79,
95%CI [1.12 – 2.85], p=0.015).