ATLAS BASED AUTOSEGMENTATION OF ORGANS AT RISK IN GYNAECOLOGICAL CANCER
PO-1334
Abstract
ATLAS BASED AUTOSEGMENTATION OF ORGANS AT RISK IN GYNAECOLOGICAL CANCER
Authors: Paolo Caricato1,2, Sara Trivellato1, Elisa Bonetto1, Valeria Faccenda1,2, Denis Panizza1,3, Stefano Arcangeli4,3, Sofia Meregalli4
1ASST Monza, Medical Physics Department, Monza, Italy; 2University of Milan, Department of Physics, Milan, Italy; 3University of Milan Bicocca, School of Medicine and Surgery, Milan, Italy; 4ASST Monza, Department of Radiation Oncology, Monza, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Accurate segmentation
of organs at risk (OARs) and target volumes is crucial for radiation treatment
planning but highly time-consuming. One commercially available solution is
atlas-based auto-segmentation (ABAS, Elekta, Stockholm). Its use aims to reduce
time-consumption and inter- and
intra-observer’s variability, which may significantly affect dosimetric
parameters. The purpose of this study was to investigate the use of ABAS in gynecological clinical routine.
Material and Methods
This feasibility study
retrospectively selected 23 patients treated with external beam radiation
therapy (EBRT) between 2019 and 2021. Ten out of 23 structure sets were used to create an atlas
library in ABAS containing bladder, rectum, and femoral heads carefully defined
by two skilled radiation oncologists. The remaining 13 patient CTs were used to
test the library performances. The following contour comparison was performed
using the Hausdorff distance (HD), the Mean Distance to Agreement (MDA), the
Dice similarity Index (DI), and the Jaccard Index (JI). The results were compared performing the
Wilcoxon Mann Whitney test to assess statistical significance (α=0.05).
Results
The auto-segmentation
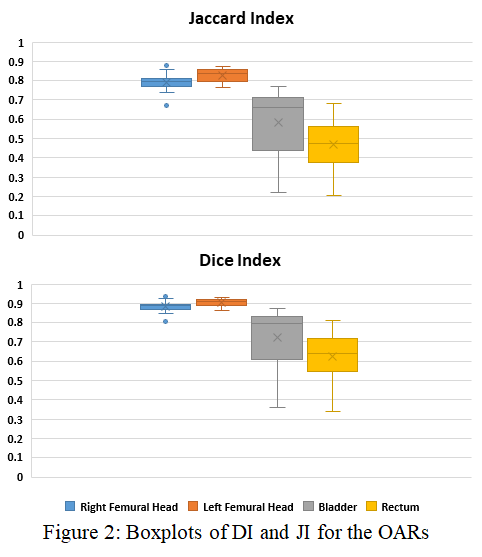
process required about 6 minutes for each CT set. Figures 1 and 2 show the geometrical metric results.
The median HD, MDA, DI, and JI values for the right femoral head were 7.44 mm
[3.66 – 17.77 mm], 1.20 mm [0.67 – 2.12 mm], 0.89 [0.80 – 0.93], and 0.80 [0.67
– 0.88], retrospectively; for the left femoral head were 7.53 mm [3.87 – 15.54
mm], 1.13 mm [0.74 – 1.39 mm], 0.91 [0.86 – 0.93], and 0.84 [0.76 – 0.87]. On
the other hand, median metric values for the bladder were 20.64 mm [12.00 –
34.95 mm], 3.13 mm [1.93 – 11.21 mm], 0.80 [0.36 – 0.87], and 0.66 [0.22 –
0.77], respectively. Lastly, the median metric results for the rectum were
23.79 mm [14.81 – 42.56 mm], 3.58 mm [2.19 – 9.98 mm], 0.64 [0.34 – 0.81], and
0.47 [0.21 – 0.68], respectively. The data comparison showed comparable ABAS
performances in rectum and bladder segmentation (p > 0.05) and in right and
left femoral heads (p > 0.05). A significant difference was registered for ABAS
segmentation performances in bilateral-femoral heads compared to rectum and
bladder (p << 0.05).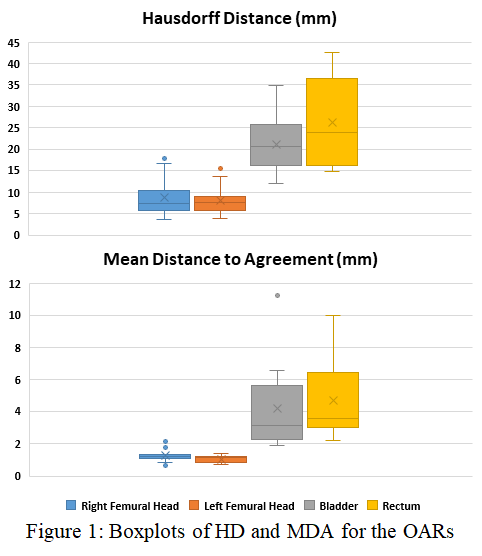
Conclusion
In these results, ABAS-bilateral-femoral heads segmentation showed higher performance compared to ABAS-bladder and ABAS-rectum segmentation because the significant bone density interface could help ABAS in femoral head delineation. Although in some cases the auto-segmentation still required manual corrections, its implementation in daily clinical practice could change the physician workflow increasing the consistency and the time-saving.