The median age
was 58 years old, male predominant (72.4%) and most (89.8%) with moderately
differentiated histology. 19.4% of all patients were T2 stage (n =19), 73.5% were
T3 stage (n = 72) and 7.1% were T4 stage (n=7). The median initial CEA concentration was 4.7 ng/dL.
All patients
completed CRT either with 50Gy in 25 fractions or with 50.4Gy in 28 fractions,
to whole pelvis and pelvic lymph nodes. The neoadjuvant chemotherapy regimen
included oral UFUR/ Capecitabine (n=72, 73.4%), FL/FOLFOX/FOLFIRI (n=8, 8.2%),
and CapeOX(n=18, 18.4%). All patients received surgical intervention in 12
weeks, after finishing RT.
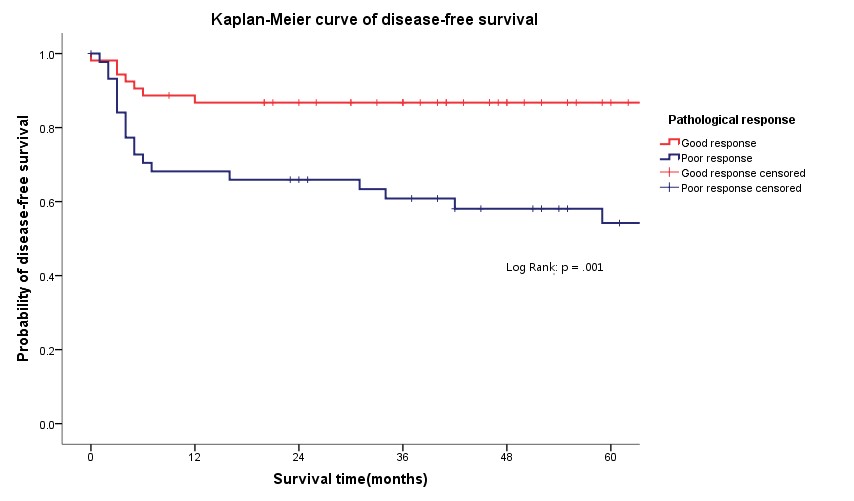
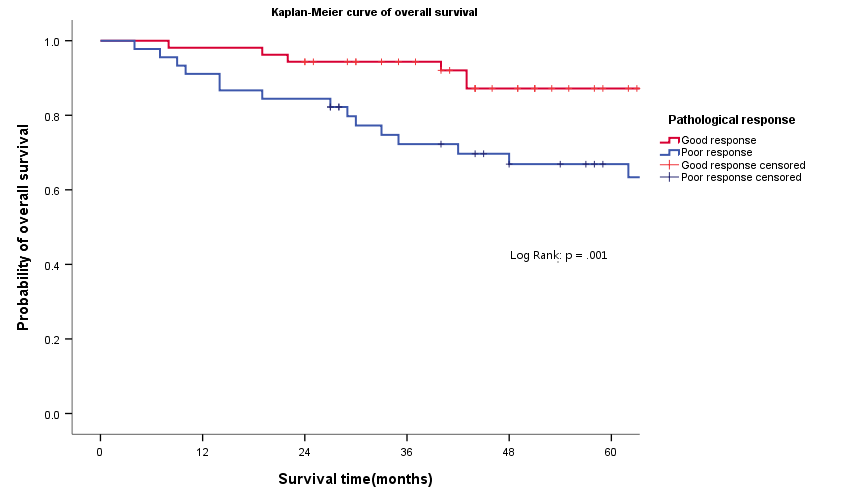
54%(n=53) of all patients
were good responders, while 46%(n=45) were poor responders. The 3-year overall
OS was 87.6% for the good responders, 70.8% for the poor responders,
respectively ( p = .001). The 3- year overall DFS was 86.8% for the good
responders, 59.3% for the poor responders, respectively ( p = .001).
Predictors of
good response on univariate LR, included volumetric modulated arc therapy (VMAT)
use, RT with simultaneous integrated boost (SIB) with a CTV_H dose over 52Gy to
gross tumor, higher CTV_H dose and an initial CEA concentration <5.0ng/mL. On
multivariate LR, RT with SIB with a CTV_H dose over 52Gy to gross tumor ( OR 9.692;
95% CI 2.791-33.660; p = .000) and pre-treatment CEA level <5.0ng/mL (
OR 0.172; 95% CI 0.058-0.509; p = .001) remained significantly associated
with good pathologic response.