Prospective assesment of quality of life before, during and after CRT in patients with anal cancer
PO-1328
Abstract
Prospective assesment of quality of life before, during and after CRT in patients with anal cancer
Authors: Frederik Fuchs1, Michael Hoffmann1, Maya Rottler1, Gretha Goesmann1, Falk Roeder2, Sabine Gerum2, Maximilian Niyazi1, Claus Belka1, Franziska Walter1
1Department of Radiation Oncology, University Hospital, LMU Munich, Munich, Germany; 2Department of Radiation Oncology, Landeskrankenhaus, Paracelsus Medical University Salzburg, Salzburg, Austria
Show Affiliations
Hide Affiliations
Purpose or Objective
Combined chemoradiotherapy (CRT) with fluorouracil (5FU) and
mitomycin (MMC) represents standard of care for patients with locally advanced non-metastatic
anal cancer and offers good 5 year survival rates up to 90%. In 02/19 we
initiated a observational study assessing the treatment tolerability as well as
quality of life before, during and after CRT. We present a planned interim
analysis.
Material and Methods
Patients receiving a CRT (VMAT, 1,8/2,2 to 45/55Gy + 2 cycles
of 5FU/MMC) as a defintive therapy for anal cancer at the University hospital
LMU, Munich were included in this study. Follow up was performed according to the
internal hospital standard. Additionally quality of life before, during and
after CRT was systematically assessed using the EORTC questionnaires QLQ-C30,
QLQ-CR29, the Wexner-, and LARS score.
Results
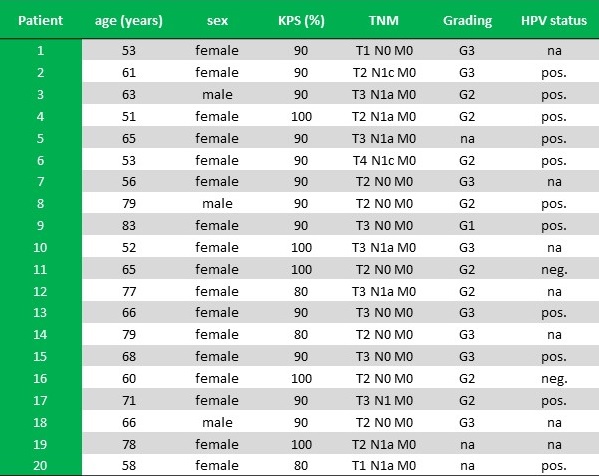
Between February 2019 und August 2021 20 patients were
included (17 female, 3 male) in this prospective study. Patient and tumour
characteristics are displayed in Table 1. The median Follow-up was 15 (2-30) months.
Distant metastases without local recurrence occured in 2 patients, both of
which died. 18 patients are currently free of disease.
Radiotherapy was carried out without interruptions in all
patients. Chemotherapy was applied with reduced dose in 6 patients due to acute
toxicity. After end of CRT dermatitis I°/II°/III° CTCAE was diagnosed in 4/11/5
patients. Diarrhea I°/II°/III° CTCAE was reported in 5/11/2 patients and fecal
incontinence I°/II°/III° CTCAE in 2/3/0 patients.
The overall response rate for the patient questionnaires was
95%/90%/90%/79%/88%/69% at the time of start of CRT/end of CRT/6 weeks/3
months/6 months/12 months after end of CRT.
Median patient reported quality of life were 6 points (range:
1 = very poor to 7 = excellent) before the initiation of therapy, 3 points at
the end of CRT and 5/6/6/6 points 6 weeks /3 Months /6 months /12 months after end
of therapy.
Conclusion
Our planned interim analysis shows a good compliance to the
questionnaire-based assessment of quality of life before, during and after CRT.
There was a significant reduction in quality of life under therapy, but also a
quick recovery already 6 weeks after end of therapy.