Chemoradiotherapy-treated anal cancer patients radiomics-based stratification to predict DSS.
PO-1317
Abstract
Chemoradiotherapy-treated anal cancer patients radiomics-based stratification to predict DSS.
Authors: Viola De Luca1, Luca Boldrini1, Stefania Manfrida1, Sara Reina2, Davide Carano3, Roberto Gatta4, Claudio Votta1, Luca Tagliaferri1, Fabio Marazzi1, Silvia Mariani2, Brunella Barbaro5, Vincenzo Valentini6, Maria Antonietta Gambacorta6
1Fondazione Policlinico Universitario A. Gemelli IRCCS, Radiation Oncology, Rome, Italy; 2Università Cattolica del Sacro Cuore, Radiation Oncology, Rome, Italy; 3Università Cattolica del Sacro Cuore, Radiology, Rome, Italy; 4Università degli Studi di Brescia, Clinical and Experimental Sciences, Brescia, Italy; 5 Fondazione Policlinico Universitario A. Gemelli IRCCS, Radiology, Rome, Italy; 6 Fondazione Policlinico Universitario A. Gemelli IRCCS, Radiation Oncology, Rome, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Although definitive chemo-radiotherapy (CRT) approach results in a high rate of disease control in anal cancer, efforts are being made to move from one treatment “fits-for-all” toward a direction of an increasingly personalized treatment, that should be tailored to specific patient and tumor characteristics through the use of quantitative imaging biomarkers. The aim of this study is to evaluate whenever radiomics predict 2-years disease specific survival (DSS) in locally advanced squamous anal cancer patients, who underwent exclusive concurrent radical CRT.
Material and Methods
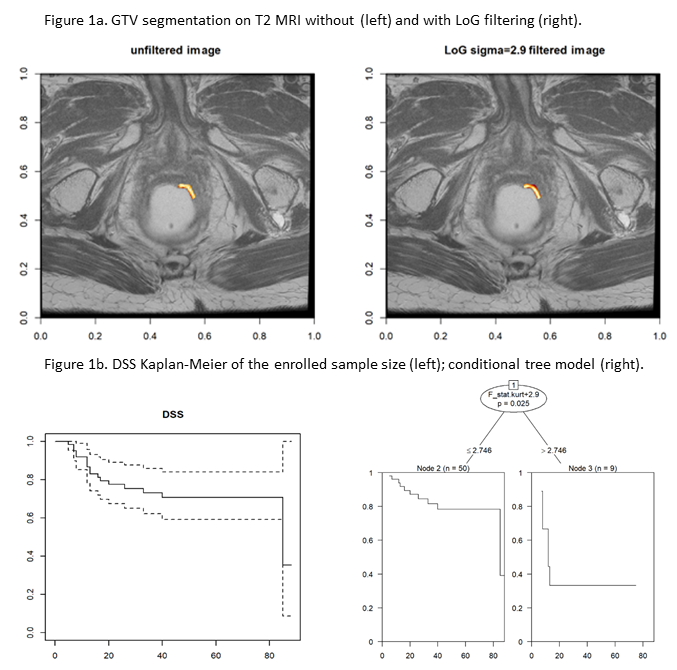
We analyzed the consecutive patients treated at our Institution between August 2011 and September 2019, whose characteristics are illustrated in Table 1. Treatment consisted of concomitant CRT with IMRT/VMAT technique and a Simultaneous Integrated Boost (SIB), eventually followed by an EBRT/brachytherapy boost. Median dose to primary tumor was 55 Gy (range 41.80 – 55.80 Gy). Median overall treatment time was 91.5 days. 2 years-DSS was considered as primary outcome of the prediction. The Gross Tumor volume (GTV) was manually segmented on the staging 1.5 T T2 MRI images for all the patients (figure 1a). A LoG filter was applied (σ 0.5-3.5 with 0.05 step) and radiomics features were extracted for all possible σ values using MODDICOM.
Results
A cohort of 64 patients (34% males, 66% females) was enrolled. Median age at diagnosis was 65.6 years (range 43-87.8). 5 patients (8%) were HIV+. Two image sets were discarded due to pixel spacing inconsistency. 14030 features spatial dimension were obtained. A cross correlation matrix was set up in order to reduce features collinearity and spatial dimension (p Pearson <0.3). From the original 14030 features space, 3 features were lastly selected (F_stat.kurt+2.9; F_cm.joint.avg+3.1 and F_cm_merged.joint.entr+3.1) and a conditional tree model to identify which feature better separates the Kaplan Meier curves at the Log Rank test.F_stat.kurt+29 appeared to be the best performing feature, and its best threshold level was identified as 2.746 (p=0.025). Figure 1b reports the curves linked to the proposed values.
Conclusion
Radiomics based patients stratification may be of help in prediction DSS in anal canal cancer patients, prioritizing treatments personalization and follow up programs. Thanks to the positive obtained results, studies on external independent cohorts are ongoing to validate the identified biomarker and additionally, studies combining radiomics and clinical features are needed.