Impact of blood parameters and normal tissue dose on overall survival in esophageal cancer patients
PO-1304
Abstract
Impact of blood parameters and normal tissue dose on overall survival in esophageal cancer patients
Authors: Esther Troost1, Laura Häberlein2, Rebecca Bütof3, Christina Jentsch1, Fabian Lohaus1, Sebastian Makocki1, Chiara Valentini1, Steffen Löck4
1University Hospital Carl Gustav Carus, Radiotherapy and Radiation Oncology, Dresden, Germany; 2Technische Universität Dresden, Faculty of Medicine, Dresden, Germany; 3OncoRay – National Center for Radiation Research in Oncology, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Helmholtz-Zentrum Dresden - Rossendorf, Dresden, Germany; 4German Cancer Consortium (DKTK), Partner Site Dresden, German Cancer Research Center (DKFZ), Heidelberg, Germany, Dresden, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
Patients with locally advanced esophageal cancer are treated with neoadjuvant radiochemotherapy (RCTx) and resection. Despite technological advances, sufficient normal tissue sparing during radiation treatment planning is still challenging. The aim of this study was thus to investigate the association of the radiation dose applied to lungs and heart as well as of various blood parameters collected before and during RCTx on overall survival.
Material and Methods
This retrospective study included 125 patients who received RCTx between 01/10 and 01/19. Patients were irradiated with photons or protons to a total dose of 40-41.4 Gy in 20 to 23 fractions and received guideline-based concurrent chemotherapy. On FDG-PET/CT, acquired for staging and treatment planning, the lungs and heart were contoured as organs at risk. From the radiation treatment plans, the mean dose (Dmean) of the lungs and heart as well as the volume of the lungs receiving more than 20 Gy (lung V20Gy) were extracted. Absolute and differential values of blood samples [hemoglobin value (Hb), platelet and leukocyte counts] pre-treatment and in the 4th week of treatment were also included in the analysis. Univariate Cox regression was used to examine the impact of these variables on overall survival, with p-values ≤ 0.05 considered statistically significant.
Results
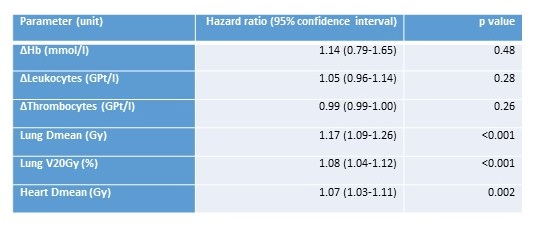
Most of the patients were male (90%), and the median age was 61 years (range: 40-79 years). Histologically, the majority of carcinomas were represented by squamous cell carcinomas (66%) as there were less adenocarcinomas (34%) amongst the patients. The median follow-up time of patients was 19.8 months (range: 0.8-91.9 months). Median overall survival measured from the start of RCTx was 37.4 months (95% confidence interval: 15.9-58.9 months). During the follow-up period, 35 patients died from esophageal cancer and 27 died for non-tumor related causes. In univariate analysis, higher normal tissue dose to lungs and heart were associated with decreased overall survival (Dmean lung: p<0.001; V20Gy: p<0.001; Dmean heart: p=0.002). None of the blood parameters was predictive of overall survival.
Conclusion
In patients with locally advanced esophageal cancer treated with RCTx, the normal tissue dose to the heart and lungs was associated with overall survival. The influence of the cardiac dose on morbidity and mortality requires further analysis in this tumor entity.