Acute toxicity associated to hypofractionation vs. standard fractionation in lung cancer treatment
Macarena M. Teja Ubach,
Spain
PO-1275
Abstract
Acute toxicity associated to hypofractionation vs. standard fractionation in lung cancer treatment
Authors: Macarena M. Teja Ubach1, Mercedes González Cantero1, María Isabel Garrido Botella1, Marta Rodríguez Roldán1, Áurea Manso de Lema1, Raúl Matute Martín1, Isabel Rodríguez Rodríguez1, Elísabet González del Portillo1, Rosa Morera López1
1Hospital Universitario La Paz, Oncología Radioterápica, Madrid, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Main objective:
to compare acute toxicity between a cohort treated with standard fractionation
and a cohort treated with hypofractionated radiotherapy.
Secondary objectives: to compare acute toxicity grade
between cohorts. To compare acute toxicity and acute toxicity grade in a
subgroups analysis: concomitant vs. no concomitant chemotherapy; Small-Cell
Lung Cancer (SCLC) vs. Non-Small-Cell Lung Cancer (NSCLS); stage; age >65 vs.
≤65 years old, radiotherapy technique 3D-CRT vs. IMRT. To evaluate if there is
any association between different variables and acute toxicity in the whole
sample.
Material and Methods
Acute toxicity assessed by Common Terminology
Criteria for Adverse Events version 4.0 (CTCAE v4.0) was retrospectively
compared between two cohorts of non-metastatic lung cancer patients. Cohort 1
(treated between April 2020 and April 2021): hypofractionated radiotherapy
(NSCLC: 55Gy/20 fractions, concurrent chemotherapy; 52,5Gy/15 fractions without
concurrent chemotherapy; SCLC: 40,05Gy/15 fractions). Cohort 2 (treated between
March 2019 and March 2020): standard fractionation (60-66Gy, 1,8-2Gy/fraction
with or without concurrent chemotherapy). Chi-square, Fisher exact test, Student-t
test, relative risk and logistic regression were used in the statistical
analysis.
Results
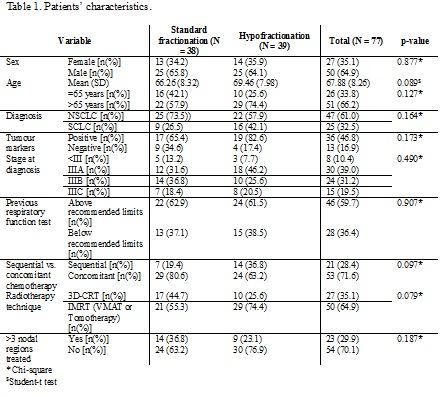
77 patients were included. Median age was 67,88
years (±8,26). 64,9% of patients were men and 35,1% were women. The most frequent
histology was NSCLC (61%) and most patients were stage III at the diagnosis
(IIIA 39%; IIIB 31,2%; IIIC 19,5%) (Table 1). In cohort 1, 24 patients had grade
1-2 toxicity, 3 patients had grade 3 toxicity and 1 patient presented grade 5
toxicity (pneumonitis). In cohort 2, 27 patients had grade 1-2 toxicity, 2
patients had grade 3 toxicity and there were no grade 4-5 toxicities. There
were no statistically significant differences neither in acute toxicity between
the two cohorts (RR 0,884 (95% CI 0,512-1,529; p=0,651)) nor in the toxicity grade
presented (RR 0,878 (95% CI 0,560-1,379; p=0,576)). No statistically
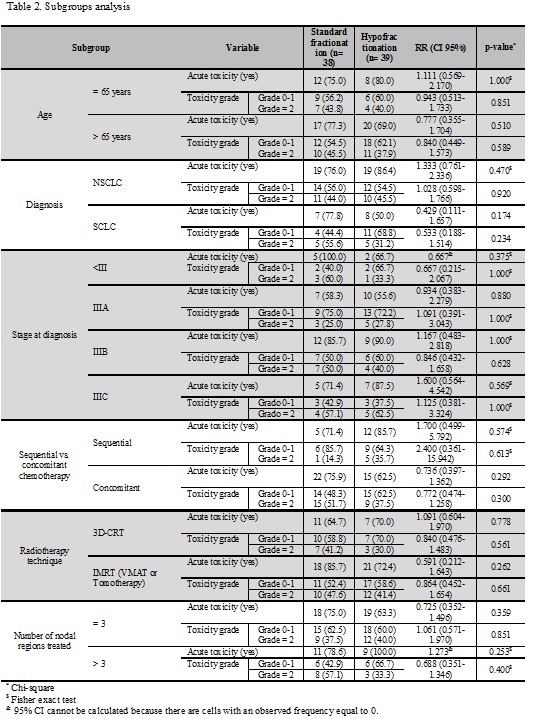
significant differences were observed in the subgroups analysis (Table 2). The
logistic regression showed that treatment on ≥3 nodal regions was independently
associated with acute toxicity.
Conclusion
In our study there were no statistically
significant differences in acute toxicity incidence between fractionation
regimens. No differences were observed in terms of acute toxicity grade neither
between the two cohorts nor in the subgroups analysis. This is concordant to
the results obtained in other retrospective studies. However, clinical trials
are needed to prospectively compare standard fractionation vs.
hypofractionation and also to compare different hypofractionated regimens. Late
toxicity and efficacy are needed to be evaluated. This and other international
studies may lay the foundations to develop clinical trials