Lung metastases from different primary tumors treated with Stereotactic ablative radiotherapy
Jady Vivian Rojas Cordero,
Spain
PO-1253
Abstract
Lung metastases from different primary tumors treated with Stereotactic ablative radiotherapy
Authors: Jady Vivian Rojas Cordero1, Gemma Sancho Pardo2, Katarina Majercakova2, Pedro Gallego Franco3, Pablo Carrasco de Fez3, Ana María Soto Cambres4, Josep Balart Serra2, Núria Farré Bernadó2
1Hospital Santa Creu i Sant Pau, Radiation Oncology, Barcelona, Spain; 2Hospital de la Santa Creu i Sant Pau, Radiation Oncology, Barcelona, Spain; 3Hospital de la Santa Creu i Sant Pau, Radiophysics, Barcelona, Spain; 4Hospital de la Santa Creu i Sant pau, Radiation Oncology, Barcelona, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
To evaluate
the clinical efficacy of stereotactic ablative radiotherapy for all lung
metastases from different primary tumors.
Material and Methods
This is a restrospective
study of patients with lung metastases from different primary tumor histologies
treated with SABR between January 2013 and September 2020.
Inclusion study criteria was:
oligometastases, oligoprogression, oligopersistance, not suitable for surgery, maximum
tumor diameter ≤ 50 mm and a maximum of 4 lung metastases. Pretreatment
evaluation was performed with 18-F-FDG PET/CT scan. Histological confirmation was performed
when feasible. Risk-adapted fractionation was used (5x11Gy,5x10
Gy,8x7.5Gy). Local control (LC),
cancer specific survival (CSS) and overall survival (OS) were retrospectively evaluated using
Kaplan-Meier method. A Multivariate analysis of variance was performed to
assess possible prognostic factors, such as dose, primary
tumor, disease-free interval, SUVmax
post-treatment PET/CT evaluation.
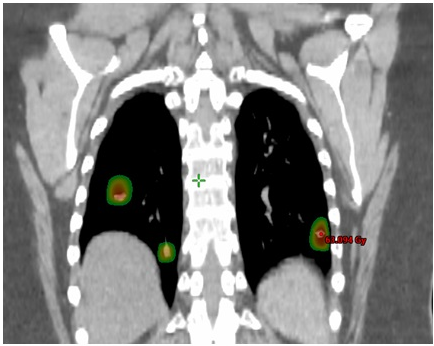
Fig 1. Patient with colorectal cancer with 3 lung nodules treated with SABR.
Results
A total of 110
nodules of 80 patients were irradiated. Median follow-up was 42 months. Median
age was 75 years (range 24-94). Median tumor size was 1.5 cm (range 0.5-4.5
cm). 74.5% were peripherals and 25.5% were central nodules. Pathologically
confirmed metastases were 16. A total of 79 tumors were oligometastases, 10
oligopersistence, and 21 oligoprogressive. According to primary tumor: Lung
cancer 30 patients (37%), Colorectal cancer 29 patients (36.25%), Soft tissue
tumors 7 patients (8.7%), Head & neck cancer 6 patients (7%) and other
histologies 8 patients (8.75%). Median total
dose was 53.9 Gy.
At 3 years
follow-up: in lung cancer LC was 94.4%, OS 69.4% and CSS 77.7%. in colorectal
cancer: LC 63.6%, OS 72%, CSS 75%, soft
tissue tumors LC of 90%, OS and CSS 72% and in Head & neck cancer LC was100%
and CSS 81% (see table 1). There was no significant difference in prognostic
factors in multivariate analysis.
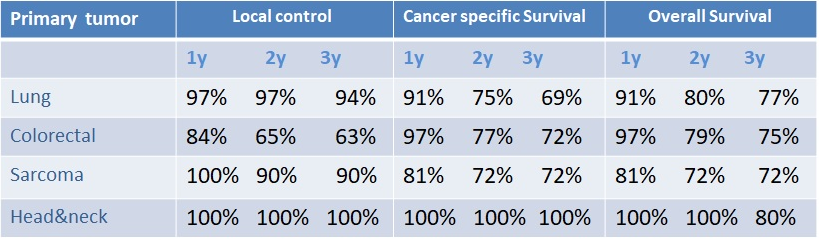
Table 1. Survival data at 1, 2 and 3 years
Conclusion
Our study
showed an excellent LC, CSS and OS for all primary tumors. Comparatively, LC remains lower in colorectal cancer and the
lowest OS at 3 year was observed in lung cancer. Further studies need to be
performed to specify the possible prognostic factors.