“Radiotherapy for Thymic Epithelial Tumors: What Is The Optimal Dose? A Systematic Review.”
PO-1240
Abstract
“Radiotherapy for Thymic Epithelial Tumors: What Is The Optimal Dose? A Systematic Review.”
Authors: Antonio Angrisani1,4, Ruud Houben1, Florit Marcuse2, Monique Hochstenbag2, Jos Maessen3, Dirk De Ruysscher1, Stephanie Peeters1
1MAASTRO Clinic, Maastricht University Medical Center, GROW school for Oncology and Developmental Biology, Department of Radiation Oncology, Maastricht, The Netherlands; 2Maastricht University Medical Center+, Department of Pulmonology, Maastricht, The Netherlands; 3Maastricht University Medical Center+, Department of Cardiothoracic Surgery, Maastricht, The Netherlands; 4University of Campania "L. Vanvitelli" , Department of Precision Medicine - Radiation Oncology Unit, Naples, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Current guidelines on radiotherapy (RT) dose for thymic epithelial tumors
(TET) based on old and small studies using 2D-RT with low levels of evidence IV-V (1). We aim to shed light on the
optimal RT doses for TET patients treated with modern RT techniques through a
systematic review of more recent literature.
Material and Methods
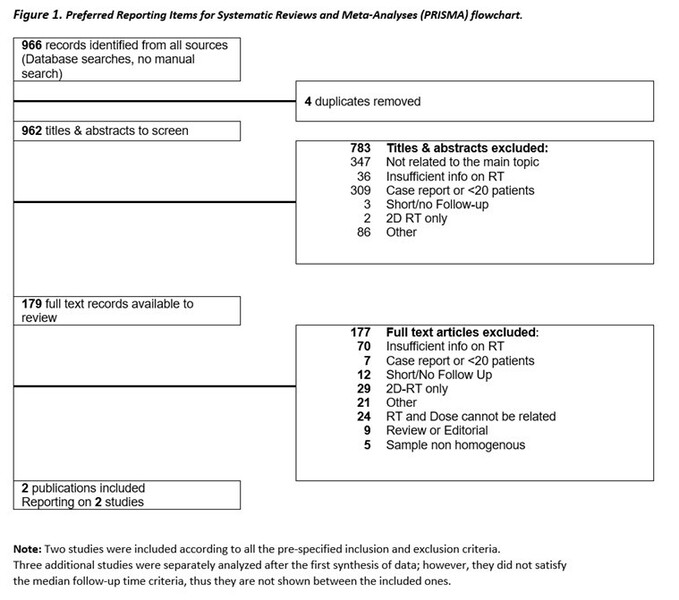
We first designed and registered the protocol (PROSPERO ID:
CRD42021241826) for review and followed PRISMA guidelines. A comprehensive
search of 4 databases was conducted. The literature search included
retrospective and prospective studies on humans affected by TETs undergoing
external beam radiation with modern techniques such as IMRT/VMAT, SBRT, 3D-CRT,
or proton therapy, published in English from 1990-2021. Inclusion criteria were
information on RT dose-response, a sample size of ≥ 20 patients, follow-up time
of ≥ 5 years, and treatment outcomes (overall survival, progression-free
survival, toxicity). Duplicates, reviews and studies reporting only 2D-RT were
excluded. Two researchers (AA, SP) independently screened and reviewed all
citations, after an interrater-reliability-test (Cohen’s Kappa). A 3rd person
(DR) provided final arbitration if consensus on inclusion could not be reached.
Risk of bias assessment was done for the selected studies using the New
Castle-Ottawa scale. AA and SP independently extracted all the data, and a
narrative synthesis without meta-analysis of the collected data was carried
out.
Results
The online database search identified 966 citations, and 179 of these were
selected for a full-text review (Fig. 1). Interrater reliability test based on
66 abstracts showed a very high agreement between the investigators (Cohen’s K
= 0,91). Only two studies fulfilled all inclusion criteria. With a less stringent minimal follow-up time of
3 years, 3 additional studies could be included. These
5 studies with a total of 357 patients were synthesized according to stage,
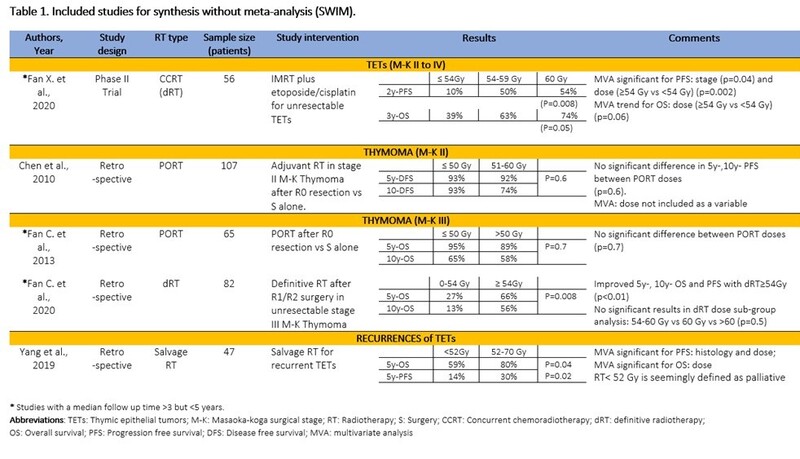
histology, and intervention (Table 1). Only 1 prospective study was found, including
patients of all stages and histology (Fan X. et al, 2020) which showed a better
OS and PFS with RT dose ≥60Gy using IMRT and concurrent chemotherapy. A
retrospective study on postoperative RT (PORT) in stage II thymoma showed no
significant results when PORT doses were compared (Chen et al, 2010). For stage
III TET, 2 studies were found: for primary or definitive RT (dRT) an improved
OS was found with a total dose of 54 Gy or higher (Fan C. et al, 2020), but not
for PORT (Fan C et al, 2013). One study on salvage RT in recurrences showed a
significantly better OS and PFS with ≥52 Gy compared to <52Gy (Yang et al,
2019).
Conclusion
With
this systematic review, we could not identify the optimal RT dose for
postoperative, nor primary RT in the era of modern RT because only a few small
studies with heterogeneity regarding WHO subtype, stage and treatment could be
identified. The question regarding the optimal RT dose to deliver for TETs is
left unanswered and warrants further research.