Deformable image registration for breast cancer radiotherapy
Marciana Nona Duma,
Germany
PO-1236
Abstract
Deformable image registration for breast cancer radiotherapy
Authors: Marciana Nona Duma1, Lea Pargmann1, Markus Böhm2, Andrea Wittig1
1Jena University Hospital, Department of Radiotherapy and Radiation Oncology, Jena, Germany; 2Jena University Hospital, Institute for Medical Statistics, Computer Science and Data Science (IMSID), Jena, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
Consistent deformable image registration (DIR) is the first step for reliable
dose deformations. The current study aimed to test whether a commercially
available DIR algorithm can reproducibly and consistently deform structures
within the same patient between free breathing (FB) and deep inspiration breath
hold (DIBH) breast cancer patients datasets.
Material and Methods
The study includes 73 patients diagnosed with left sided breast cancer
with CTs in FB and DIBH. Breast clinical
target volumes (CTV) according to ESTRO, the heart, the left anterior
descending artery (LAD), both lungs were contoured in FB and DIBH in the
RayStation (RaySearch Laboratories, Stockholm, Sweden). DIR was performed
taking the structure set of the FB to be deformed on the DIBH (FB→DIBH) and
vice versa (DIBH→FB). Further, DIR was performed focusing on the whole image
(“no focus”- DIR_none), the CTV (DIR_CTV), the heart (DIR_heart) or on the surgical
clip in the tumor bed (DIR_clip), respectively.
Volume differences (∆V) and a dice similarity index (DSI) were calculated.DSI= 2xCV / (mROI_V+dirROI_V);
CV- common volume of mROI_V and dirROI_V;
mROI_V - manually contoured region of interest volume;
dirROI_V - by DIR automatically generated volume.
Generalized estimating equations were used to assess the statistical
effect of the different DIR focuses on the DSI.
Results
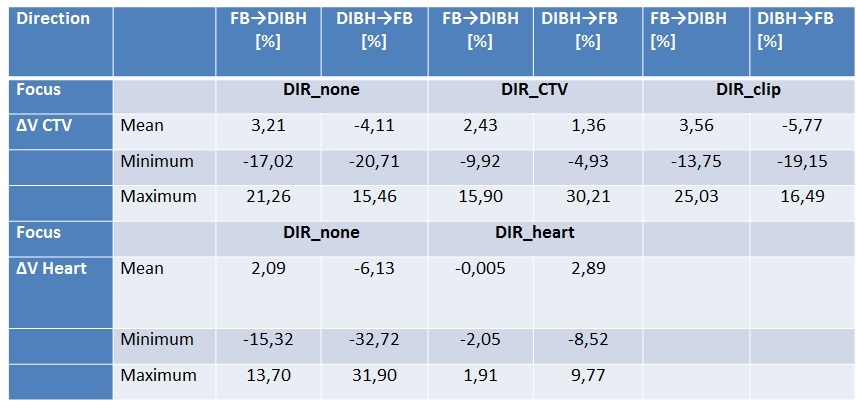
Table 1 depicts the volume differences (∆V in %) between manually and
automatically contoured structures exemplary for the CTV breast and the heart.
The highest DSI for the CTV was achieved by DIR_CTV (p<0.05) regardless
of DIR direction (FB→DIBH or DIBH→FB); there was no statistical difference between
DIR_clip and DIR_none for the DSI CTV. The DSI of the heart was the highest
when focusing on the heart. There are no significant effects of breast size on
DSI CTV_breast, ∆V breast left or ∆V heart. Patients with smaller breasts
achieved higher DSI of the heart compared to those with larger breasts. By
every inhaled 100cm³ the DSI CTV_breast would increase by 0.05 (p<0.05). In
contrast the DSI heart would decrease by 0.002 (p<0.05) for every inhaled 100cm³.
Conclusion
The individual anatomy of the patient - such as breast volume or amount
of deep inspiration – have an impact on DIR accuracy. DIR of the whole image is
not enough for precise volumetry of organs and implicitly dose deformations
between FB and DIBH datasets. Performing focused DIR is an option.