Radiotherapy-based management of non-metastatic Inflammatory breast cancers: a retrospective study
PO-1229
Abstract
Radiotherapy-based management of non-metastatic Inflammatory breast cancers: a retrospective study
Authors: Benjamin Nicaise1, Pierre Loap1, Fatima Laki2, Delphine Loirat3, Jean-Yves Pierga3, Alain Fourquet1, Youlia Kirova1
1Institut Curie, Radiation Oncology, Paris, France; 2Institut Curie, Surgery, Paris, France; 3Institut Curie, Medical Oncology, Paris, France
Show Affiliations
Hide Affiliations
Purpose or Objective
Inflammatory
breast cancer (IBC) is a rare clinicopathological presentation of breast cancers
(BC) characterized by diffuse tumor emboli in dermal lymphatic vessels. IBC have
a poor prognosis compared with non-inflammatory BC, and treatment of
non-metastatic IBC usually includes neo-adjuvant chemotherapy (NACT), followed
by total mastectomy and adjuvant radiotherapy (RT). This retrospective study
aims to describe the clinical outcomes of non-metastatic IBC patients treated
with this multidisciplinary approach
Material and Methods
This
single-center retrospective study included all women diagnosed
with non-metastatic IBC between 01/2010 and 01/2018 at the Institut Curie and
treated with NACT, surgery and RT. Overall survival (OS), disease free survival
(DFS) and locoregional free survival (LRRFS) were calculated from time of
diagnosis. Prognostic factors for patient survival were analyzed based on
univariate and multivariate regressions.
Results
113 pts were
treated for a non-metastatic IBC with NACT, RT with or without surgery (Table
1). Median age was 51 yrs, 79.7% of pts had N+ tumors, median Ki67 was 40%,
60.2% had grade III tumors; triple-negative breast cancers (TNBC) represented
34.6% of cases. A large majority of pts (91.2%) received adjuvant post-mastectomy
RT (Table 2) and only ten pts (8.8%) received pre-operative RT; 17 pts (15%)
received concomitant chemo-radiotherapy (mostly with 5FU-vinorelbine). Surgery
was conducted in all but one patient (97.3%) and usually consisted of a total
mastectomy (96.5%) with an axillary dissection (96.5%). Non-pCR was observed in
76 pts (67.3%). Radiotherapy delivered a median dose of 50 Gy to the breasts or
the chest wall in 25 fractions; Berg’s level I, II-III, IV and internal mammary
chains were included in 21.2%, 88.5%, 89.4% and 85% of all patients
respectively. While the majority were treated with 3D technique, 11 pts were
treated with rotational IMRT (VMAT or helical tomotherapy).
With a median
follow-up of 54 months, 5-year OS, DFS and LRRFS were 78% [CI: 70.1-86.8%],
68.1% [59.6%-77.7%] and 85.2% [78.4%-92.7%] respectively. In multivariate
analysis, non-pCR was an adverse prognosis factor for OS, DFS and LRRFS;
pre-operative RT was an adverse prognosis factor for OS and DFS; TNBC and N+
disease were adverse prognosis factors for OS. Radiation-related adverse events
were limited to acute skin toxicity (22% of grade 2 and 2% of grade 3
dermatitis); no late radiation-induced toxicity was reported.
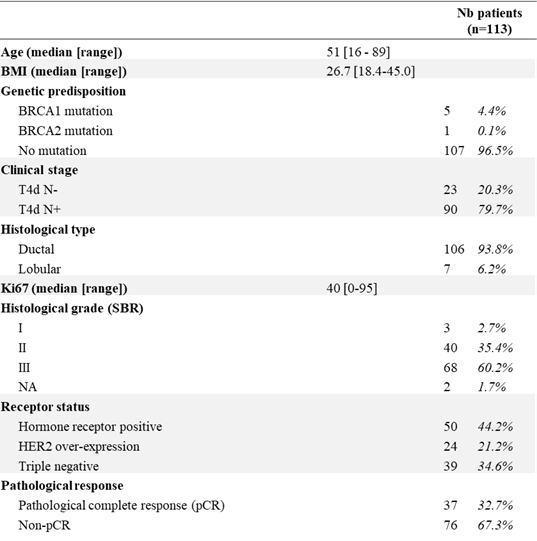
Table 1:
patient characteristics.
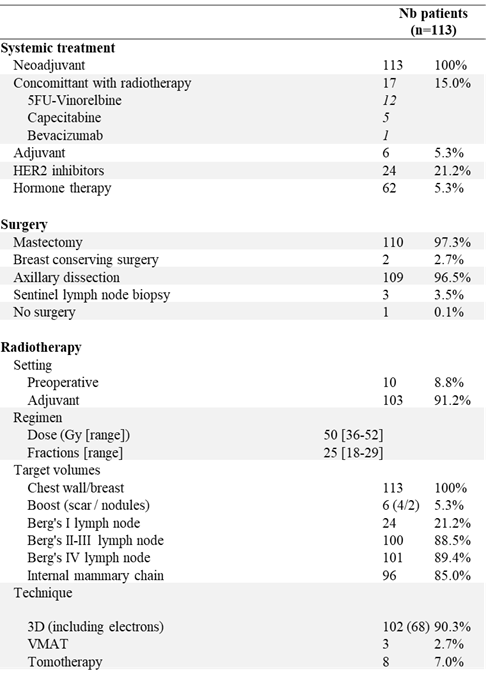
Table 2: Treatment
characteristics.
Conclusion
High locoregional control could be achieved with multidisciplinary
management of non-metastatic IBC, suggesting the anti-tumor efficacy of
radiotherapy in this rare but pejorative clinicopathological
presentation. While comparing favorably with historical cohorts, OS and
DFS could be potentially improved in the future with the use of new
systemic treatments, such as PARP-inhibitors or immunotherapy.