Thirty-two consecutive
patients for a total of 82 metachronous HER2- BCBM
treated with CyberKnife were included in this preliminary analysis.
Median follow up from
primary surgery and SRS was 113 months (range 42-241) and 17 months (range
0-101).
Median time to
brain-progression from initial diagnosis of breast cancer was 78 months (range:
15-215) with 17/32 (53%) patients with both cranial and controlled-extracranial
disease at the time of of SRS.
Patients were treated for
all brain lesions they presented, with a median of 2 lesions for each patient
(range, 1 – 9). Total median SRS dose was 21 Gy (range, 18 -24 Gy) given in 1
to 3 fractions, in alternate days. Median single lesion GTV was 0.29 cm3
(range, 0.02 – 13.22).
At the last follow up
available, 17/32 patients were alive (OS=53% ; 16 patients with both cranial
and extracranial disease).
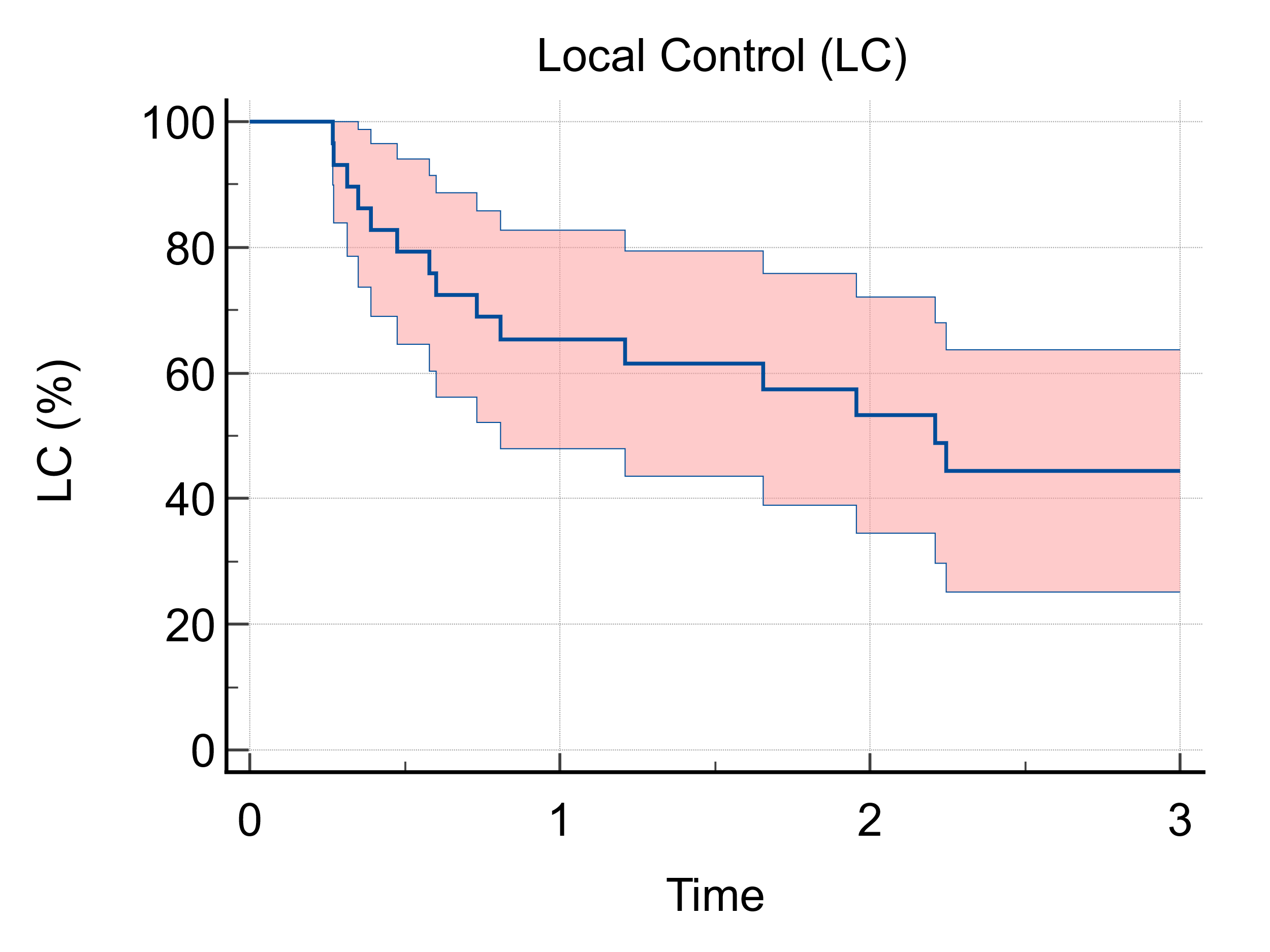
LC was reported in 56 of the
82 treated lesions (68%; 1 and 3-years LC : 65% and 45%, respectively-Fig 1), while DBC (no appearance of any
new intracranial lesions) was observed in 10/32 patients (31%).
Univariate and multivariate analysis
for correlation with demographics, tumour and treatment characteristics are
ongoing.
No patients
experienced severe neurotoxicity (Grade 4-5 in the Common Terminology Criteria
for Adverse Events) with only 5 asymptomatic radionecrosis recorded.