Outcomes following hypofractionation to nodal region after surgery in locally advanced breast cancer
Riccardo Ray Colciago,
Italy
PO-1193
Abstract
Outcomes following hypofractionation to nodal region after surgery in locally advanced breast cancer
Authors: Riccardo Ray Colciago1, Francesco Tramacere2, Stefano Arcangeli1, Raffaella Lucchini1, Francesco Pati3, Maurizio Portaluri3
1School of Medicine and Surgery – University of Milan Bicocca, Department of Radiation Oncology, Milano, Italy; 2ASL A. Perrino, Department of Radiation Oncology , Brindisi, Italy; 3 ASL A. Perrino, Department of Radiation Oncology, Brindisi, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
In daily clinical practice,
there are concerns about the potential toxicity of hypofractionated (HF)
post-mastectomy radiation therapy (PMRT) and regional nodal irradiation (RNI).
In this retrospective study, we aimed to analyze the impact on outcomes and toxicity of a 3-week HF
schemes after axillary dissection and breast surgery (quadrantectomy or
mastectomy), to assess its safety and efficacy in patients with locally
advanced breast cancer (BC).
Material and Methods
Eligible patients were women
with stage IIA – IIIC pathologically confirmed invasive BC who underwent
axillary dissection and breast surgery (conservative or mastectomy) including
patients who underwent breast reconstruction or received neoadjuvant or adjuvant
systemic therapy.
Two different
hypofractionation schedules were allowed: 40.05 Gy in 15 fractions over 3 weeks
and 42.56 Gy in 16 fractions daily, both with an optional sequential boost of
10 Gy in 4 fractions. RT was delivered using 3D planning techniques. Using
Kaplan-Meier survival procedure, loco-regional recurrence (LRR), distant
metastases free survival (DMFS) overall survival (OS) and acute and late
toxicities were analyzed.
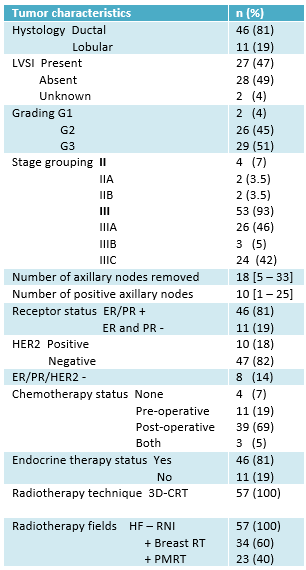
Results
57 patients with a median
age of 60 years old (32 – 85) were retrospectively analyzed. Fifty-three women
(93%) had stage III BC, whose 24 (45%) were stage IIIC. All patients underwent
axillary dissection along with breast conservative surgery in 34 (60%) cases
and with radical mastectomy in 23 (40%) cases; 4 (7%) patients had surgical
reconstruction. Thirty-four (60%) patients underwent HF RT to whole breast plus
regional nodal irradiation (RNI) and 23 (42%) patients received HF
post-mastectomy RT plus RNI.
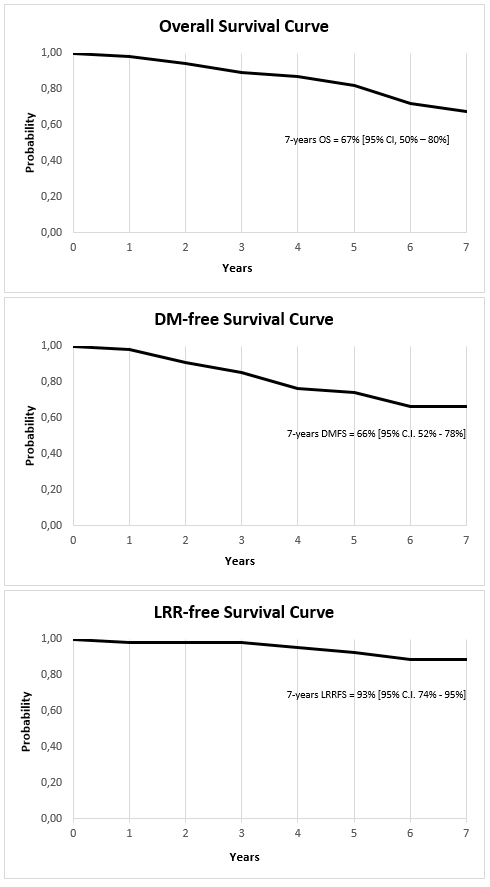
At a median follow-up of 80
months (30 – 113), the combined loco-regional recurrence rate was 7% and the
7-year LRR-free survival was 93% (95% Confidence Interval [CI], 74% - 95%).
Sixteen patients (28%) developed distant metastasis, of which 8 (50%) were
bone, 3 (19%) were parenchymal and 5 (31%) both. The 7-year DMFS was 76% (95%
CI, 52% - 78%). Death Occurred in 12 (22%) patients. The 7-year OS was 67% (95%
CI, 50% – 80%). Grade 1 and grade 2 acute skin toxicity occurred in 19 (35%)
and 9 (16%) patients, respectively. No grade 2 and grade 3 late skin toxicity
have been observed in all patients. Late arm lymphedema was reported in 12
(21%) women, with arm impairment in 8 (75%) cases.
Conclusion
Our findings show that loco-regional HF RT after
axillary dissection and breast surgery in patients with locally advanced breast
cancer was safe and effective. Longer follow up is needed to empower analyses
on late toxicity and clinical outcomes. More randomized trials are needed to
achieve strong evidence on the use of these fractionations