The impact of RT on oligorecurrent BC: a retrospective analysis of predictors of clinical outcome
PO-1181
Abstract
The impact of RT on oligorecurrent BC: a retrospective analysis of predictors of clinical outcome
Authors: Alessia Casbarra1, Samuele Frassoni2, Cristiana Fodor3, Annamaria Ferrari3, Raffaella Cambria4, Francesca Colombo1, Jessica Franzetti1, Carlotta Giandini1, Ilaria Repetti1, Vincenzo Bagnardi2, Silvia Della Pasqua5, Marco Colleoni5, Maria Cristina Leonardi6, Barbara Alicja Jereczek-Fossa1
1IEO, European Institute of Oncology IRCCS; University of Milan, Division of Radiation Oncology; Department of Oncology and Hematoncology, Milan, Italy; 2University of Milan-Bicocca, Department of Statistics and Quantitative Methods, Milan, Italy; 3IEO, European Institute of Oncology IRCCS, Division of Radiation Oncology, Milan, Italy; 4IEO, European Institute of Oncology IRCCS, Unit of Medical Physics, Milan, Italy; 5IEO, European Institute of Oncology IRCCS, Division of Medical Senology, Milan, Italy; 6IEO, European Institute of Oncology IRCCS,, Division of Radiation Oncology, Milan, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
A growing interest has recently raised around the role of radiotherapy (RT) as metastases-directed therapy (MDT) on clinical outcomes of patients affected by oligorecurrent disease. In the current study, we addressed oligometastatic breast cancer (OMBC) patients, who after primary tumor control, developed oligorecurrent disease to evaluate how RT on all metastases affected survival outcome compared to RT to only some lesions.
Material and Methods
Consecutive oligorecurrent BC patients irradiated on oligometastatic sites at the European Institute of Oncology IRCCS between 2011 and 2019 were considered for the analysis. Oligometastatic status was defined as the presence of five or fewer metastases in two or fewer organs, including brain. Patients were categorized in two subgroups, one where all the metastatic sites were irradiated (ablative group) and one where only some of the lesions were irradiated with symptomatic intent (palliative group). Patients’ and clinical information were collected from electronic medical records, focusing on RT details and treatment related toxicities. Outcomes included overall survival (OS), progression free survival (PFS), local control (LC), measured starting from RT delivery. Univariate (UVA) and Multivariate (MVA) analysis were performed.
Results
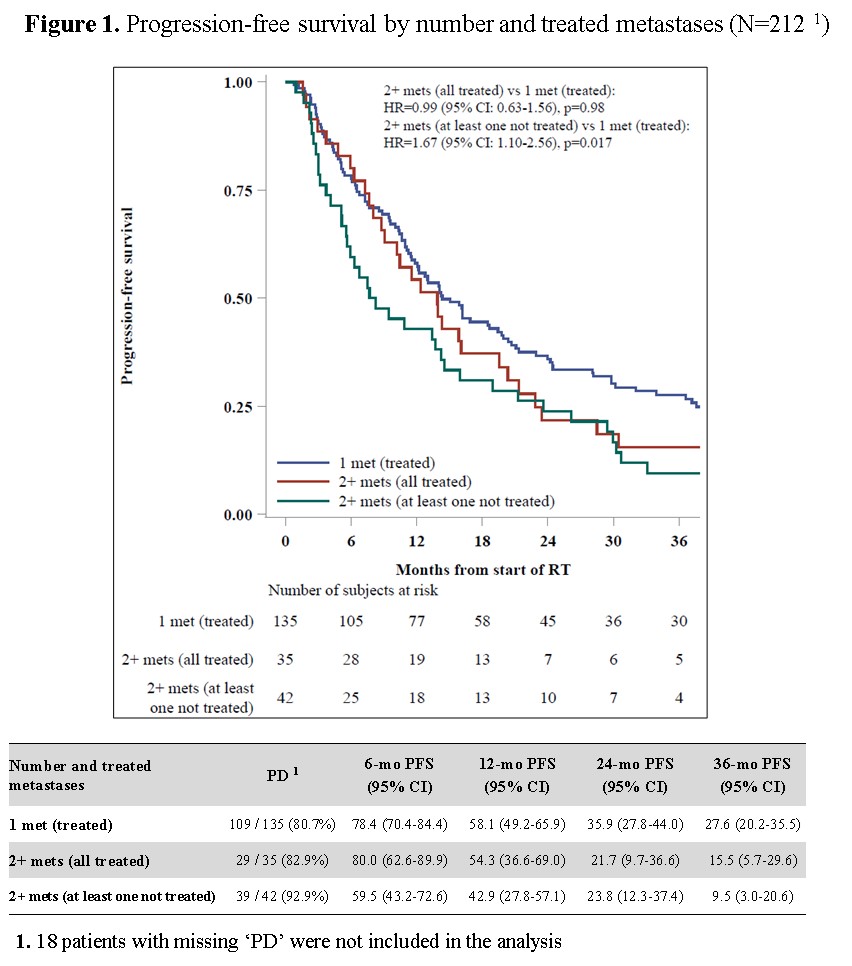
A group of 230 oligorecurrent BC patients, with 300 lesions, was analyzed. The most common molecular subtype of the primary tumor was Luminal A (41.7%). The most common metastatic site was bone (62.4%). Lesions were treated with conformal-3D-CRT (41.8%), stereotactic radiation therapy - SRT (40.1%) and intensity-modulated RT- IMRT (18.1%). Median prescribed dose was 30 (8-55) Gy resulting in a median BED of 56.3 (24-297) Gy. The ablative group consisted of 185 women, of whom 146 presented only one and 39 two or more lesions, while the palliative group was formed of 45 subjects, in which 77 lesions remained untreated. LC was obtained in 259 lesions (92%). No ≥ grade 2 toxicity was observed. Four patients developed complications (three bone fractures and one ischemic event). Median PFS was 13.9 months. At 12 months, PFS was 54.4% and at 24 months was 31.2%. At UVA and MVA, triple negative subtype and the palliative intent resulted to be statistically significant predictors for worse PFS. In fact, having two or more lesions of which at least one not irradiated compared to having 2 or more lesions all irradiated brought the 12-month PFS from 42.9% to 54.3% and the 36-month PFS from 9.5% to 15.5%, respectively (Fig. 1). Median OS was 6 years. The OS at 2 years was 83.9%, while
it dropped at 54.3% at 5 years. No difference in OS emerged between the two groups. At UVA and MVA, only older age and poor performance status were statistically significant predictors.
Conclusion
Our analysis showed that RT is a safe MDT with high rates of LC. While OS was not influenced, delivering RT with ablative intent, to all the metastatic lesions, significantly improved PFS.