Low-dose radiotherapy for extranodal marginal zone lymphoma of bronchus-associated lymphoid tissue
PO-1170
Abstract
Low-dose radiotherapy for extranodal marginal zone lymphoma of bronchus-associated lymphoid tissue
Authors: Morgan Freret1, Brandon Imber1, Erel Joffe2, Joachim Yahalom1, Carla Hajj1
1Memorial Sloan Kettering Cancer Center, Radiation Oncology, New York, USA; 2Memorial Sloan Kettering Cancer Center, Medical Oncology, New York, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
Primary extranodal marginal zone lymphoma of bronchus-associated lymphoid tissue (BALT) has an indolent clinical course, and optimal treatment strategies at diagnosis are not well established. Retrospective analyses show equivalent or superior outcomes with surgical resection compared to systemic therapy or active surveillance, however the role of radiotherapy in disease management remains underexplored. Here we evaluated outcomes among nine consecutive patients with primary BALT lymphoma treated with radiotherapy (RT) to test the hypothesis that RT is associated with favorable local control and survival outcomes.
Material and Methods
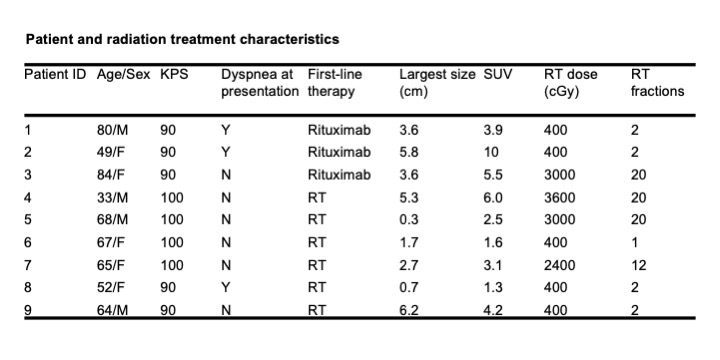
We retrospectively reviewed records for 28 patients with marginal zone lymphoma involving the lung treated at a single institution between 2000 and 2021, of which 9 met criteria for study inclusion. Inclusion criteria included age ≥18 years, disease confined to the lungs and hilar and/or mediastinal lymph nodes, and lack of concurrent malignancy. We calculated progression-free (PFS) and overall survival (OS) using the Kaplan-Meier method.
Results
The median follow-up was 27 months (range, 10 – 176 months). Six patients had newly diagnosed BALT lymphoma, and three patients were treated for progressive disease after rituximab. All patients except for one with bilateral lung involvement received tumor-limited fields with a median dose of 4 Gy (range, 4 – 36 Gy). The majority of patients (n = 5) received low-dose RT with 4 Gy. The 5-year PFS rate was 100%; the median PFS from RT was not reached. The median OS from RT was 124 months. Of 9 treated patients, only one went on to develop recurrent disease in a portocaval lymph node. There were no cases of local recurrence and no reported RT-related toxicities.
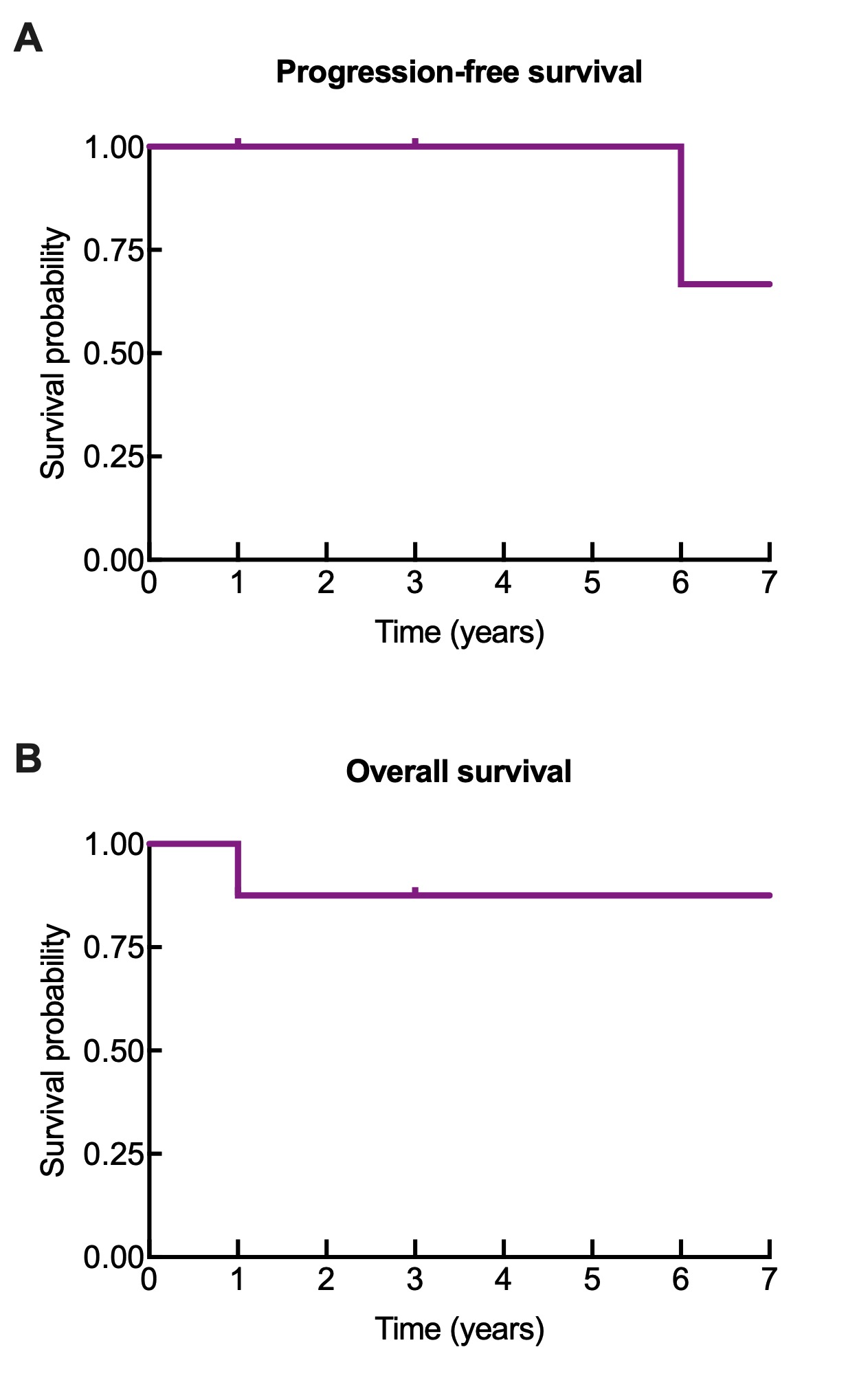
Conclusion
Radiotherapy, including low-dose radiotherapy, for localized primary BALT lymphoma is associated with excellent progression-free and overall survival outcomes with no treatment-related toxicities reported in this cohort. RT represents a feasible treatment strategy that may be considered in both the recurrent and upfront treatment settings.