Re-irradiation with Stereotactic Radiotherapy for Recurrent High Grade Glial Tumors
Ela Delikgoz Soykut,
Turkey
PO-1158
Abstract
Re-irradiation with Stereotactic Radiotherapy for Recurrent High Grade Glial Tumors
Authors: Ela Delikgoz Soykut1, Eylem Odabasi1, Nilgun Sahin1
1Samsun Training and Research Hospital, Radiation Oncology, Samsun, Turkey
Show Affiliations
Hide Affiliations
Purpose or Objective
Despite the radical treatments applied, local
recurrence is encountered in the majority of high-grade gliomas (HGG). There is
no standard treatment when recurrence is detected, but stereotactic radiotherapy
(SRT) is a preferable alternative in this context. The aim of this retrospective
study is to evaluate the efficacy of SRT for recurrent HGG, and to investigate
the factors that affect survival outcomes.
Material and Methods
From
September 2013 to March 2021, a total of 59 patients with 64 lesions were
re-irradiated with CyberKnife stereotactic radiotherapy. The primary endpoints
of the study were overal survival (OS), progression free survival (PFS) and
local control rates (LCR). Survival
curves were estimated with the Kaplan-Meier method and compared using log-rank
test, hazard ratios were estimated using Cox regression
analysis.
Results
Eleven
of the patients were WHO grade 3 anaplastic astrocytomas, and 48 of the
patients were WHO grade 4 glioblastomas. All of the patients received a median
of 60 Gy (59.4-60 Gy) of postoperative radiotherapy (RT), and 51 of them
received oral temozolomide chemotherapy, concurrently. The median time to first
recurrence was 13 (4-85) months. 12 of the patients had a second surgery before
re-irradiation. SRT was performed as a median prescription dose of 30 Gy (range
15-30), with a median of 5 fractions (1–5). The median follow-up time was 4
months (range 1–57), 11 patients were alive at the last follow-up. The median OS
after re-irradiation was 8 (95% CI: 4.66-11.33) months, and 1- and 2-y OS were 33.2%
and 14.2%, respectively. In
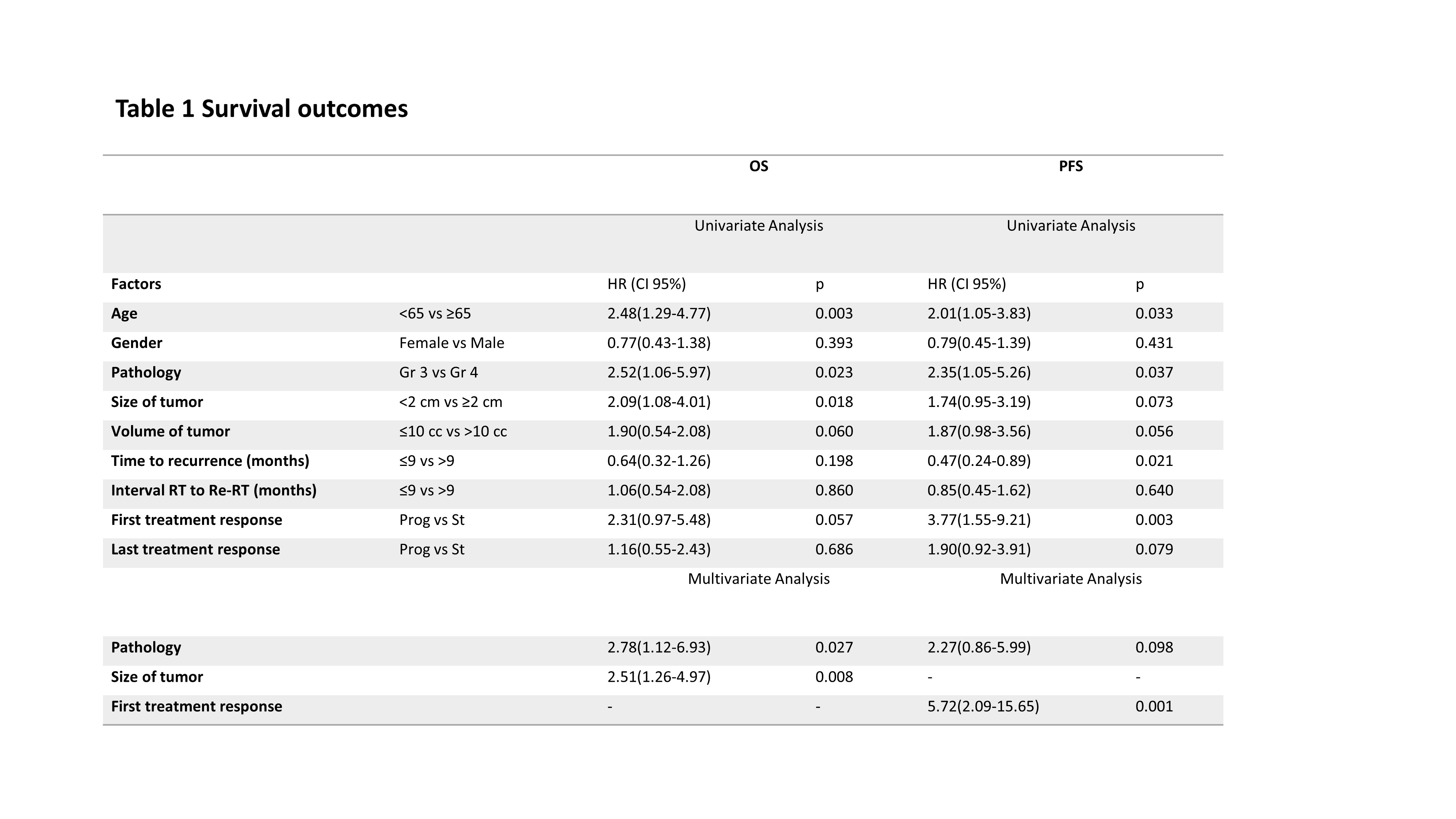
the univariate analysis, age <65 years (p =0.003), grade 3 gliomas (p =0.023),
size of tumor <2cm (p=0.018) were associated with better survival. Grade 3
gliomas (p =0.027), size of tumor <2cm (p=0.008) were remained independent
prognostic factors for OS in the multivariate analysis. Recurrence
after re-irradiation was detected in 20 patients, 6
of them belonged to new lesions. The
median PFS after re-irradiation was 5 (95% CI: 3.39-6.60) months, and 1- and 2-y PFS were 24.5% and 9.5%,
respectively. In
the univariate analysis, age <65 years (p =0.033), grade 3 gliomas (p =0.037),
stable response at first evaluation with magnetic resonance imaging (p=0.003),
and time to recurrence >9 months (p=0.021) were associated with improved PFS. Stable response
(p =0.001) was remained prognostic factor for PFS in the multivariate analysis.
LCR were 62.7% and 33.9% at the first and last follow up. There was no serious toxicity.
Conclusion
SRT is
a viable treatment modality with significant survival contribution in recurrent
HGG. It should be considered when deciding on re-irradiation during follow-up,
as it may have a favorable prognostic effect on survival in patients with tumor
size <2 cm.