Comparative planning study (IMPT vs VMAT) on sparing OARs important for neurocognition in gliomas
Laurien De Roeck,
Belgium
PO-1133
Abstract
Comparative planning study (IMPT vs VMAT) on sparing OARs important for neurocognition in gliomas
Authors: Laurien De Roeck1, Jeroen Blommaert2, Gilles Defraene2,3, Charlotte Sleurs2, Laurens Vandenbussche2, Maarten Lambrecht3,2,4
1University Hospitals Leuven, Department of Radiation Oncology, Leuven, Belgium; 2KU Leuven, Department of Oncology, Leuven, Belgium; 3University Hospitals Leuven, Department of Radiation Oncology, Leuven, Belgium; 4Particle Therapy Interuniversitary Center Leuven, Department of Radiation Oncology, Leuven, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy-induced
neurocognitive decline affects 50-90% of adult glioma survivors. Several organs
at risk (OARs) have been identified to play a role in neurocognitive
functioning. Proton therapy is expected to outperform photon therapy in sparing
many of these OARs from excess dose. In this study, we compared Volumetric Modulated
Arc Therapy (VMAT) vs Intensity Modulated Proton Therapy (IMPT) for its OAR
sparing capability in glioma patients.
Material and Methods
In this in
silico dosimetric comparison study, we included 10 glioma patients (grade II
and III astrocytoma and oligodendroglioma) who were treated to a total dose of
54-60 GyRBE. Seven tumours were located in the left hemisphere, two in the
right hemisphere and one in the brainstem. The OARs that could play a role in
neurocognitive functioning (cerebellum anterior and posterior, ipsi- and
contralateral thalamus, ipsi- and contralateral hippocampus, corpus callosum, supratentorial
brain minus CTV, brain (minus CTV)) were
delineated according to the EPTN atlas for contouring in neuro-oncology1.
For each patient, both a VMAT (2 partial arcs) and robust IMPT (2-3 beams) treatment
plan were optimized according to the same set of clinical dose constraints. Average
and near-maximum (D2%) doses in 9 OARs were extracted from the planning system
(Raystation and Eclipse). To evaluate the dose metrics of the IMPT plan, the
nominal scenario was used. To evaluate target coverage, D95% of the CTV was
used in both treatment techniques. DVH metrics from both techniques were
compared using a two-sided Wilcoxon rank-sum test with a p-value of <0,05
indicating significance.
Results
In total, 20
treatment plans were analysed (1 VMAT and 1 IMPT for each patient). A statistically
significant reduction was established using IMPT in 6 out of 21 dose metrics in
3 out of 5 OARs important in neurocognitive functioning: Dmean supratentorial
brain minus CTV (p<0,001), Dmean contralateral hippocampus (p=0,019), D40%
contralateral hippocampus (p=0,001), Dmean brain (p=0,007), Dmean brain minus
CTV (p< 0,001) and Dmean contralateral thalamus (p=0,002). The dose coverage
(D95% CTV) was not statistically different between both groups (p=0,529).
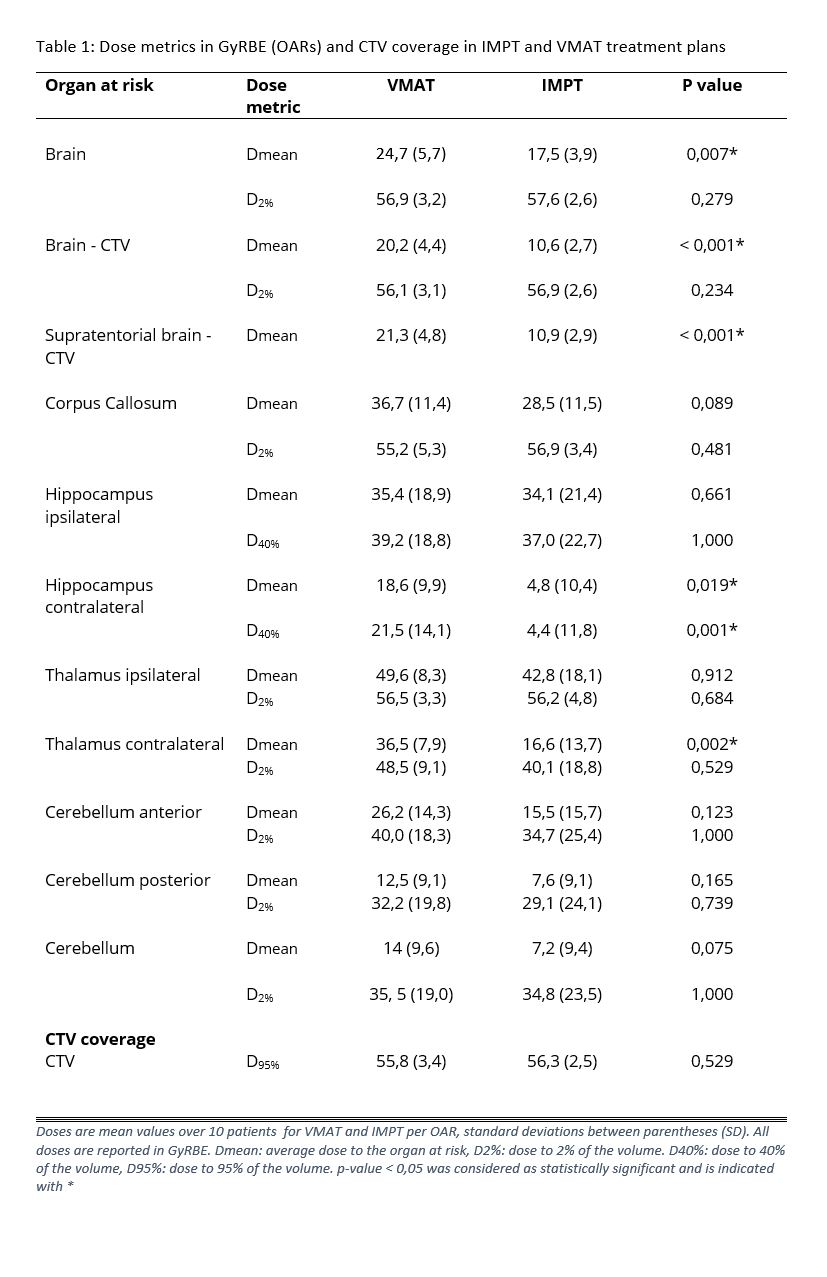
Conclusion
The use of IMPT
resulted in important OAR sparing in this glioma patient population translating
in a lower mean dose to the contralateral hippocampus, contralateral thalamus
and supratentorial brain minus CTV, and a lower D40% to the contralateral
hippocampus. To evaluate whether this translates into a clinical benefit for
these patients, we will compare the ROCOCO Performance Scoring System scores2
between both groups in a planned analysis.