Radiosurgery with Cyberknife® for arteriovenous malformations: technical and dosimetrical analysis
Esmeralda Scipilliti,
Italy
PO-1128
Abstract
Radiosurgery with Cyberknife® for arteriovenous malformations: technical and dosimetrical analysis
Authors: Esmeralda Scipilliti1, Valentina Borzillo1, Rossella Di Franco1, Federica Savino2, Giuseppe Leone3, Mario Muto3, Paolo Muto4
1Istituto Nazionale Tumori IRCSS Fondazione G. Pascale, Radiation Oncology Unit, Napoli, Italy; 2LB Servizi per le aziende SRL, Medical physics, Roma, Italy; 3A.O.R.N. Cardarelli, Department of Neuroradiology, Napoli, Italy; 4Istituto Nazionale Tumori Fondazione G. Pascale, Radiation Oncology Unit, Napoli, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiosurgery (SRS) obtain a successful obliteration
of arteriovenous malformations (AVMs). Radiation injury to the vascular
endothelium induced the proliferation of smooth-muscle cells and the
elaboration of extracellular collagen, which leads to progressive stenosis and
obliteration of the AVM nidus thereby eliminating the risk of hemorrhage. The
advantages of SRS, compared to microsurgical and endovascular treatments, are
that it is noninvasive, has minimal risk of acute complications, and is
performed as an outpatient procedure. The primary disadvantage of SRS is that
cure is not immediate; thrombosis of the lesion is achieved in most cases, but it
does not occur until 2-3 years after treatment. SRS has been shown to be less
effective for lesions over 10 cc in volume. Aim of the study is to describe a
monoistitutional series of AVMs pts treated with CyberKnife® system (CK) in
collaboration with dedicated neuroradiologist
Material and Methods
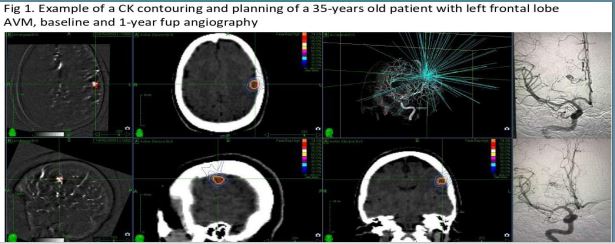
All pts performed angiography, CT-angio and
MR-angio and were evaluated by an expert neuroradiologist before CK treatment.
All imaging data were accurately co-registered in the CK-TPS and used for
target contouring delineation. The delineation of AVM targets was as follows:
AVM with prior embolization targets included nidus, embolization areas and some
small draining veins; for pts without embolization, the target was nidus. All
pts received a single fraction of radiation. The PTV was equal to GTV.
Follow-up was performed with MR-angio after 2-3 months and angiography 1 year
after the treatment
Results
From Dec 2017 to May 2021, 9 pts (4m, 5f), mean age
42 (18-56) with AVMs were treated with CK. AVMs were located within cerebellum
(3), temporal lobe (3), parietal lobe (2) and frontal lobe (1). 6 pts had
previously undergone endovascular embolization. Median GTV was 3,65 cc
(0,09-11,99) and median marginal dose was 19 Gy (18-21) with median isodose
prescription of 80% (74-85). PTV median coverage was 99,76% (97,54-100) with
median PTV CI of 1,6 (1,16-2,14). 6 pts completed the RT course, 1 pt had
asymptomatic brain radionecrosis 19 months after the RT, 5 pts had > 1-year angiographic
follow-up: 4 had stable disease and 1 AVM obliteration
Conclusion
A specialized team approach is necessary for CK
treatment of AVMs, including an SRS expert radiation oncologist and medical
physicist, and an interventional neuroradiologist. CK is safe and effective for
AVMs treatment, but long-term data are needed