Intensity Modulated Radiotherapy (IMRT) after conservative surgery for supraglottic tumours
PO-1114
Abstract
Intensity Modulated Radiotherapy (IMRT) after conservative surgery for supraglottic tumours
Authors: Daniela Alterio1, Sabrina Vigorito2, Francesca Emiro2, Maria Giulia Vincini1, Annamaria Ferrari1, Simona Marani1, Matteo Pepa1, Mattia Zaffaroni1, Cristiana Fodor1, Stefania Volpe3, Giulia Marvaso3, Luca Bergamaschi3, Cristiana Pedone3, Jessica Franzetti3, Stefano Zorzi4, Marta Tagliabue4, Mohssen Ansarin4, Barbara Alicja Jereczek-Fossa3
1IEO European Institute of Oncology IRCCS, Division of Radiation Oncology, Milan, Italy; 2IEO European Institute of Oncology IRCCS, Unit of Medical Physics, Milan, Italy; 3IEO European Institute of Oncology IRCCS, University of Milan, Division of Radiation Oncology, Department of Oncology and Hemato-Oncology, Milan, Italy; 4IEO European Institute of Oncology IRCCS, Division of Otolaryngology and Head and Neck Surgery, Milan, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Patients (pts) with locally advanced supraglottic cancers (LASGC) treated with conservative surgery (CS) followed by postoperative 3D conformal radiotherapy (3DCRT) could be affected by high rate (up to 30%) of severe long-term treatment-related side effects. Data on the impact of Intensity Modulated Radiotherapy (IMRT) in improving the toxicity profile are lacking. Aim of the present analysis was to report long-term toxicity of pts with LASGC treated with CS followed by postoperative IMRT. Dosimetric comparison between IMRT and 3DCRT was also performed.
Material and Methods
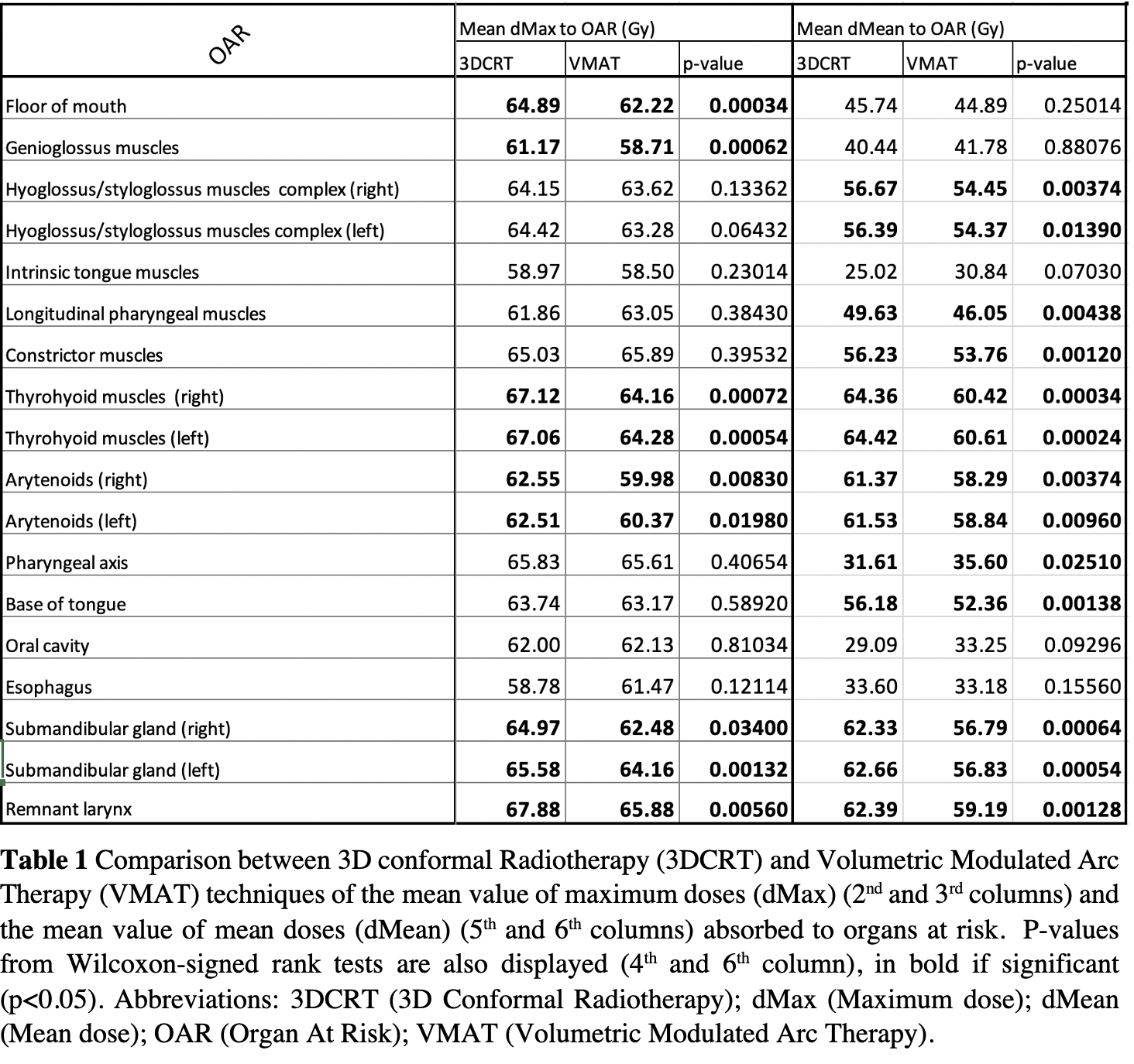
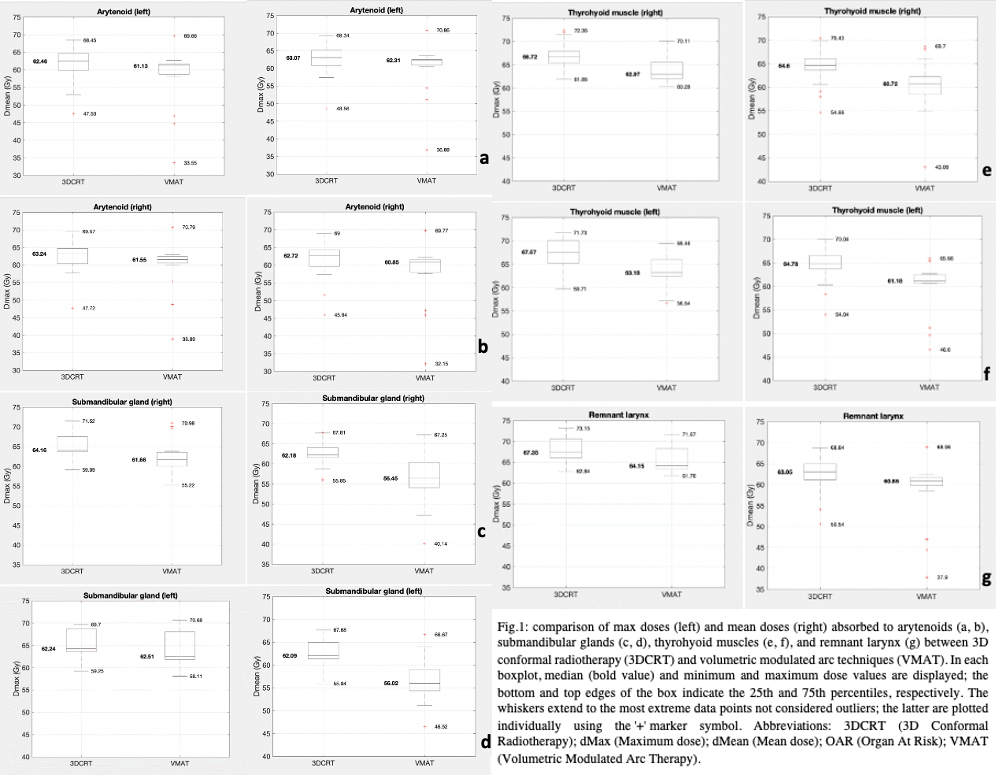
Data of pts treated from 2014 to 2020 with CS and postoperative IMRT for locally advanced (stage III and IV according to AJCC 7th Ed) cancers of the supraglottis have been prospectively collected. Exclusion criteria were: 1) early-stage (stage I and II) disease; 2) recurrent tumours; 3) previous treatments on head and neck region; 5) follow-up shorter than 6 months. Simultaneous Integrated Boost (SIB)-IMRT was performed using Volumetric Modulated Arc Therapy (VMAT) technique; to make the comparison, a 3DCRT plan was calculated for each of pts using a shrinking field technique with the same IMRT dose levels. Swallowing-related structures (SWARs) and Swallowing Functional Units (SFUs) were retrospectively contoured on each patient. Post-hoc Wilcoxon-signed-rank tests (p-value < 0.05) were used to perform a comparison between maximum and mean doses (dMax and dMean, respectively) of IMRT and 3DCRT treatment plans to assess possible differences between absorbed doses to remnant larynx (RL), arytenoids, SWARS, and SFUs.
Results
Twenty pts have been analysed. Advanced tumor (pT3/4) and advanced nodal (pN2/3) stages were found in 13 and 11 pts, respectively. Median follow-up was 33 months (range 8-92 months). At last follow up, 15 pts were alive without disease, 5 pts died (2 for progression and 3 for other causes). During the follow-up course, 5 (20%) pts required temporary tracheostomy while 2 (10%) pts required both temporary tracheostomy and enteral nutrition. At last follow up one patient (5%) had still in place both tracheostomy and percutaneous endoscopic gastrostomy (PEG). No patient had esophageal stricture and/or chondronecrosis. Results of dosimetric comparison have been reported in Table1. Both IMRT dMax and dMean resulted significant lower compared to 3DCRT technique according to Wilcoxon-signed rank test for 7 structures (LR, arytenoids, thyroid muscles, and submandibular glands); relative boxplots are displayed in Fig1.
Conclusion
Severe long-term toxicity rate of CS followed by IMRT resulted to be low and seems to compare favourably with historical data of pts treated with the 3DCRT approach. The dosimetric analysis confirmed that IMRT allows a significant reduction of absorbed doses for the majority of analyzed structures compared to the 3DCRT approach.