Hypoxia and Perfusion MR-Imaging on the MR-Linear Accelerator for Head and Neck Cancer
Amit Gupta,
United Kingdom
PO-1111
Abstract
Hypoxia and Perfusion MR-Imaging on the MR-Linear Accelerator for Head and Neck Cancer
Authors: Amit Gupta1, Wajiha Bano2, Helen Barnes3, Kate Newbold4, Chris Nutting4, Shreerang Bhide4, Kevin Harrington4, Andreas Wetscherek2, Kee Howe Wong4
1Institute of Cancer Reseasrch, Radiotherapy and Imaging, London, United Kingdom; 2Institute of Cancer Research, Radiotherapy and Imaging, London, United Kingdom; 3The Royal Marsden Hospital, Therapeutic Radiography, London, United Kingdom; 4The Royal Marsden Hospital, Head and Neck, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
The detrimental impact of hypoxia on tumour control has been well described in head and neck cancers (HNC). Tumour vasculature is morphologically abnormal, resulting in aberrant blood flow and oxygen delivery to cells.
The Elekta Unity MR-linear accelerator (MRL) allows daily MR imaging and adaptive radiotherapy with the on-board 1.5T MRI scanner.
This study aims to investigate the feasibility of performing R2* and Intra-Voxel Incoherent Motion (IVIM) sequences on the MRL to evaluate longitudinal changes of hypoxic and perfusion parameters over a course of radiotherapy in patients with HNC.
Material and Methods
Four patients with stage III (TNM 8th edition) p16-positive oropharyngeal squamous cell carcinomas received radical radiotherapy to 65 Gy in 30 fractions to the primary target and involved nodes. Patients were scanned with radial multi-echo gradient-echo and diffusion-weighted MRI sequences on the MRL at baseline pre-radiotherapy and once weekly during radiotherapy.
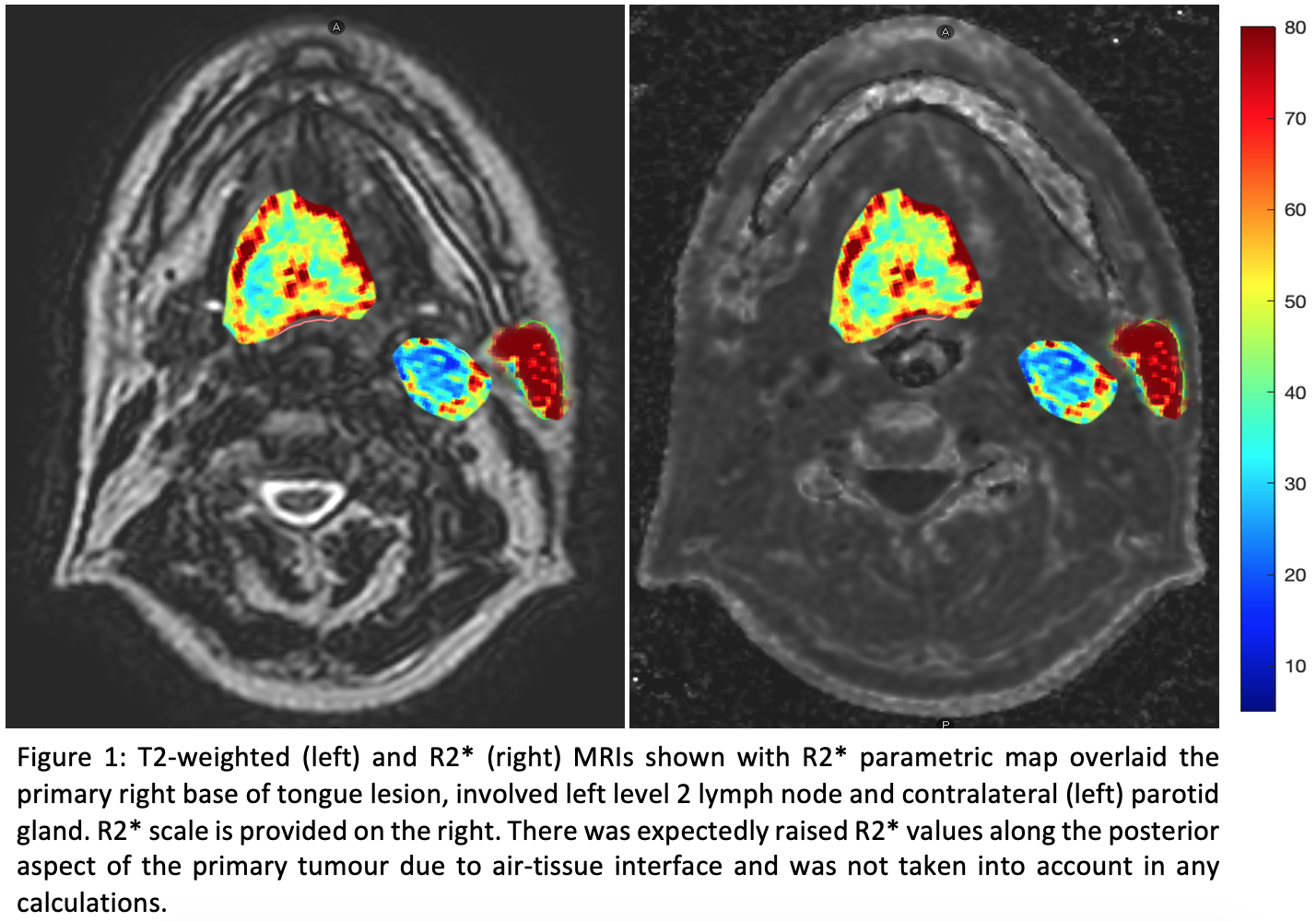
R2* maps were generated in MATLAB by calculating the linear regression of the natural log of signal intensities from the multi-echo images, on a voxel-by-voxel basis. Perfusion maps from the diffusion-weighted sequences (b0, 30, 150 and 500 s/mm²) were generated in MATLAB.
RayStation treatment planning system was used for Dicom analyses. R2* and perfusion maps were fused with T2-weighted MRIs. Primary targets and involved nodes were contoured by a radiation oncologist and histograms were generated to derive voxel-wise data. Contralateral parotid glands were used as controls and to normalise R2* data. Hypoxic voxels were defined as R2* above 60 s‾¹. “Hypoperfusion fraction” was defined as the total voxel volume of perfusion fractions between 0-15%.
Results
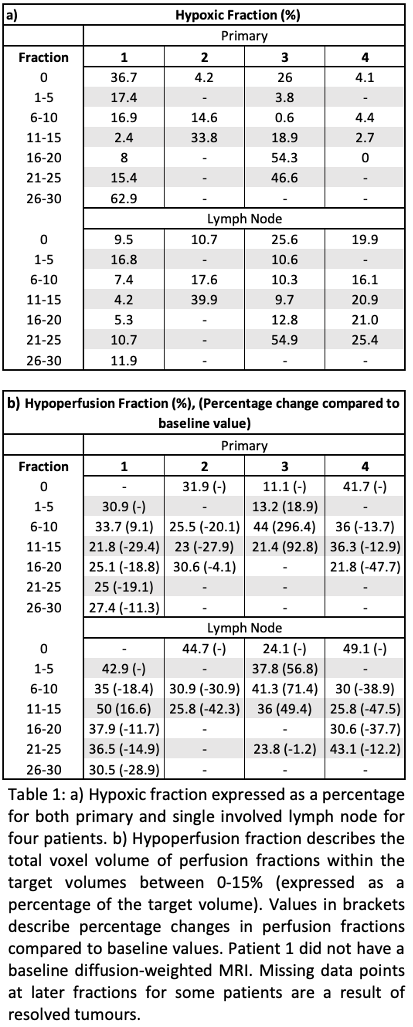
Table 1 displays the hypoxic and perfusion fractions of the primary and involved lymph nodes. An example R2* image for patient 1 is shown in Figure 1.
Patients 2 and 4 had complete resolutions of primary tumours during radiotherapy with complete responses on post-treatment FDG PET/CTs. Patients 1 and 3 had increases in hypoxic fractions towards the end of treatment and both had residual avidity on post-treatment PET/CT scans attributed to inflammation. Patient 3 had a large increase in hypoperfusion fraction of the primary (296%). Patients 1, 2 and 4 saw reductions in the hypoperfusion fractions during radiotherapy.
In lymph nodes, Patients 1 and 3 had increases in hypoxic fractions towards the end of treatment. Hypoperfusion fractions increased in patients 1 and 3. The largest increase in hypoperfusion fraction was in patient 3 (71.4%).
Conclusion
Our preliminary data show that R2* and IVIM MRIs are feasible on the MRL. This study reveals various trends in the evolution of tumour hypoxia and perfusion fractions in HNC. However, further work requires analyses of geometric and measured signal accuracies and sequence optimisation. Patient recruitment continues to establish the roles of tumour hypoxia and perfusion fraction as predictive biomarkers.