HPV Status and Fitness Associated With Aspiration Risk at One Year After Head and Neck Radiotherapy
PO-1106
Abstract
HPV Status and Fitness Associated With Aspiration Risk at One Year After Head and Neck Radiotherapy
Authors: Eliana Maria Vasquez Osorio1, Deborah Ganderton2, Azadeh Abravan1, Andrew Green1, Andrew McPartlin3
1The University of Manchester, Division of Cancer Sciences, Manchester, United Kingdom; 2North Manchester General Hospital, Head and Neck Oncology and Voice, Manchester, United Kingdom; 3The Christie NHS Foundation Trust, Clinical Oncology, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Experiencing
difficulties swallowing, or dysphagia, is a common side effect of head and neck
radiotherapy. It is experienced by more
than 80% of the patients at the end of treatment, with a significant proportion
of patients having permanent impairment of swallowing sufficient to cause
aspiration. For these patients, modification of diet, with potential requirement
for enteral feeding, is generally recommended with consequent negative effect on
long term quality of life. There is an unmet clinical need to better predict the
long-term aspiration risk during initial discussions with patients of treatment
side effects. In this study, we present
a simple model, including baseline variables to predict aspiration risk at 1
year, assessed via 100 ml water test.
Material and Methods
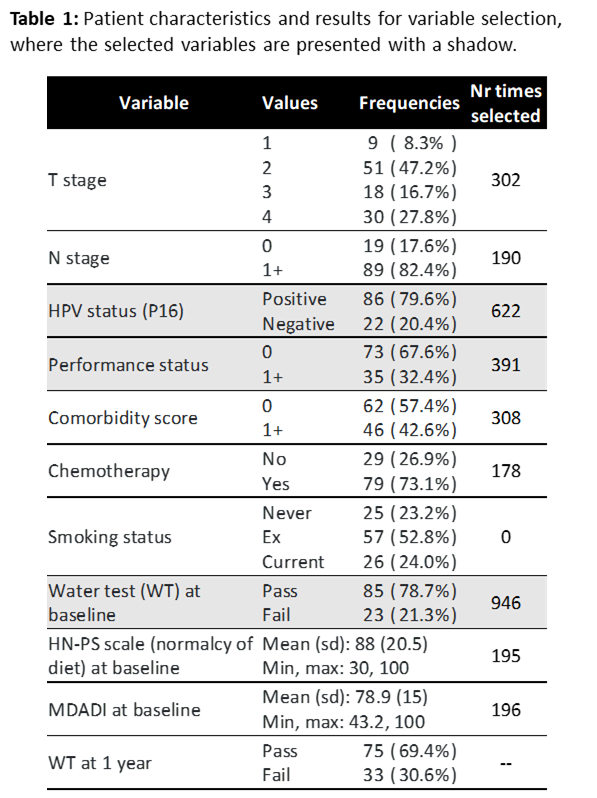
Data from 108
oropharyngeal cancer patients were collected, including baseline clinical and
tumour factors and various pre-treatment dysphagia scores: M.D. Anderson
Dysphagia Inventory (MDADI), water test (WT), performance status scale for
normalcy of diet (HN-PSS), table 1. A logistic regression predicting WT failure
(defined as the patient coughing, having a wet voice quality post swallow, or
not being able to finish the task) at 1 year was conducted. The final model was
found by performing backward variable selection with bootstrapping (keeping top
3 selected variables, n=1000) and adjusting for internal overfitting using
uniform shrinkage (based on optimism-adjusted calibration slope, n=1000). Model
performance was assessed using area under the curve (AUC) of the receiver
operating characteristic curve.
Results
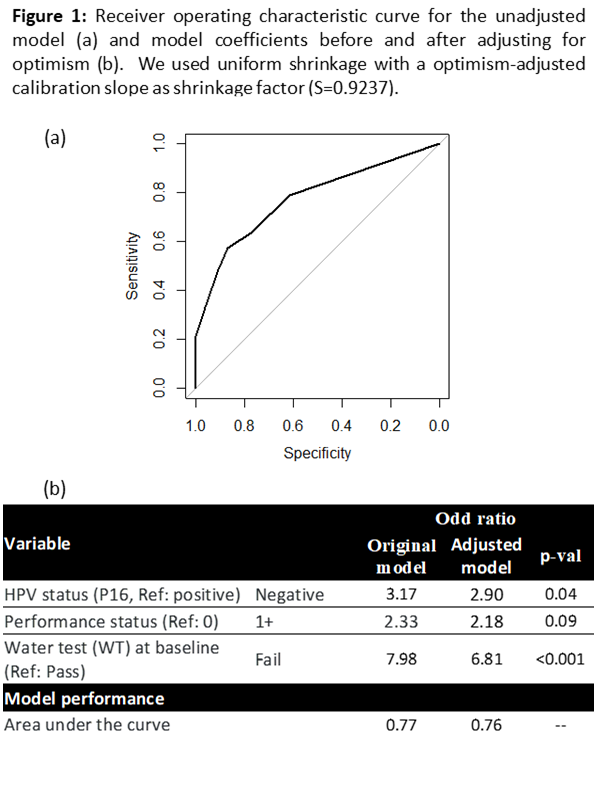
30.6% of patients
failed the water test at 1 year. Water test at baseline, HPV status (assessed
via P16), and performance status (PS) were selected for the final model (table
1 and figure 1). Performance of the model, assessed via AUC and adjusted for
optimism, was 0.76. The strongest predictor for failing water test at 1 year is
the test at base line (OR 6.8, p<0.001). Additionally, HPV negative patients
have approximately 3 times the chance of failing the test at 1 year (OR 2.9,
p=0.04), indicating possible differences in treatment toxicity trajectory.
Conversely, poorer general status (PS 1+ vs PS 0) is also associated with a
higher risk of failing the test (OR 2.18, p=0.09).
Conclusion
We propose a simple
model using only baseline variables, and corrected for overfitting, which
predicts dysphagia at 1 year (assessed via water test). Although the major
factor for failing WT at 1 year is the pre-treatment test result, it
is important to consider other factors when initially discussing treatment as
suggested by our model. We find a novel association with HPV status independent
of disease stage or location, suggesting a possible underlying variation in
response to radiotherapy related to HPV infection. After external validation,
this simple model could be used during patient consultations to personalise discussion
of possible side effects.