Results of postoperative radiotherapy in salivary gland tumors: a 10-years’ experience
PO-1103
Abstract
Results of postoperative radiotherapy in salivary gland tumors: a 10-years’ experience
Authors: Olga Engel1, Ruth Rodríguez Romero2, Raquel Benlloch Rodríguez1, Beatriz Gil Haro1, Sofía Santana Jiménez1, Sofía Córdoba Largo1, Marta López Valcárcel1, María Hernández Miguel1, Patricia Sarrión Rubio de la Torre1, Jesús Romero Fernández1
1University Hospital Puerta de Hierro, Radiation Oncology, Madrid, Spain; 2University Hospital Puerta de Hierro, Radiation Protection and Medical Physics, Madrid, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Salivary
gland tumors (SGT) are a heterogeneous group of tumors with different
histologies. Standard treatment is surgery followed by radio or
chemoradiotherapy in high-risk patient.
The objectives is to
determine overall survival (OS), local relapse-free survival (LRFS), nodal
relapse-free survival (NRFS) and distant metastases-free survival (DMFS) in
patients treated with postoperative radiotherapy (PORT).
Material and Methods
From 2010-2020, 26 patients
with SGT were treated. Mean age: 58 years (19-89). Male:15 p; female:11 p.TNM (AJCC 8th edition)
stages: I-II (11p); III (3p); IVA/B (12p). No patients had distant metastases
at the time of diagnosis. Most patients had positive margin resection (R1,
80%). Histology: ductal: 7p; mucoepidermoid: 4p; acinar cell: 4p; others: 11p.
Mean RT dose to tumor bed was 63 Gy (60-70). Neck nodes were irradiated in 22p
(17 ipsilateral, 5 bilateral). Twelve patients received cisplatin-based
concomitant chemotherapy. Statistic Kaplan-Meier, log-rank
Results
With mean follow up of 41
months (1-129) 5-year OS, LRFS, NRFS and DMFS were 48.6%, 92 %, 82.6% and
54.4%, respectively.
Patients with pT3pT4 had more
probability of vascular invasion (p=0,018) and more likely had cervical nodes
involvement (p=0,019).
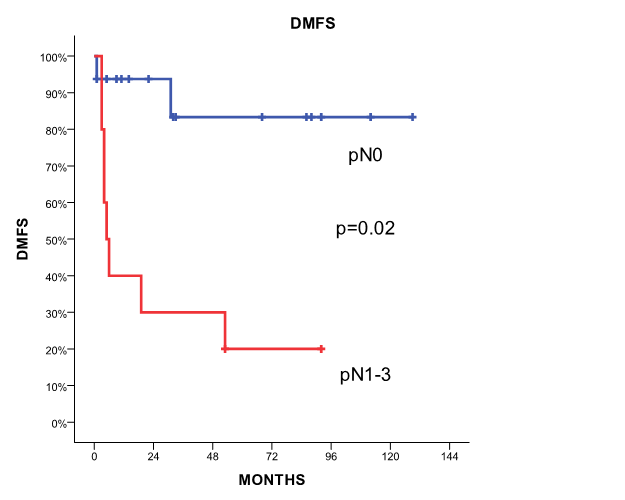
Patients with pN1-3 nodal disease had a significant
increase in distant metastases (5-y DMFS of 20% vs 83.3% for patients with pN0,
p=0.02). Patients with pN1-3 stages have a worse non-significant OS than pN0
patients (5-y OS 20.2% vs 65.7%).
Conclusion
Despite of the majority of
patients had R1 resection, local control was excellent in our series. We found
an unexpected high rate of distant metastases. The only prognostic factor that
predicts poor overall survival and distant failure was nodal pathologic stage
pN1-3. Our results open the question of the need of systemic chemotherapy for
patients with pathologically involved lymph nodes.