Impact of sarcopenia in oropharyngeal cancer patients treated with radical chemo-radiotherapy
chiara lucrezia deantoni,
Italy
PO-1100
Abstract
Impact of sarcopenia in oropharyngeal cancer patients treated with radical chemo-radiotherapy
Authors: chiara lucrezia deantoni1, Anna Chiara1, Aurora Mirabile2, Sara Broggi3, Claudio Fiorino3, Andrei Fodor1, Marcella Pasetti1, Roberta Tummineri1, Flavia Zerbetto1, Simone Baroni1, Ariadna Sanchez Galvan1, Vanesa Gregorc2, Italo Dell'Oca1, Nadia Gisella Di Muzio4
1IRCCS San Raffaele Scientific Institute, Radiation Oncology, Milano, Italy; 2IRCCS San Raffaele Scientific Institute, Department Unit of Oncology, Medical Oncology Department, Milano, Italy; 3IRCCS San Raffaele Scientific Institute, Medical Physics, Milano, Italy; 4Vita-Salute San Raffaele University, Faculty of Medicine and Surgery, Milano, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Sarcopenia
(SP), defined as loss of muscle mass and functions, recently emerged as an
independent prognostic factor in oncological patients (pts), connected with
poor survival and sometimes with a higher treatment toxicity profile. This
study aims to determine the possible impact of SP on survival and acute
toxicity in our oropharyngeal pts.
Material and Methods
76
pts with locally advanced oropharyngeal squamous cell carcinoma, stage III-IVC,
were treated in our Center with Helical TomoTherapy (HT) between 2005 and 2021.
HT was delivered with a Simultaneous Integrated Boost (SIB) technique: 54 Gy
(1.8 Gy/day) to the clinically negative neck region and 66 Gy (2.2 Gy/day) or
69 Gy (2.3 Gy/day) to the tumor and positive nodal regions based on 18FDG
CT/PET imaging. All pts received concomitant platinum-based CT (at least 200
mg/m2).
SP
is generally determined on single-slice CT measurement of the cross sectional
muscle area (CSA) at the level of the third lumbar vertebra (L3). Swartz et al
(2016) proposed and validated an algorithm that correlated CSA at L3 with CSA
at C3, easier to obtain in head and neck pts, and then CSA at C3 with lumbar
skeletal muscle index (SMI). Twenty pts (26%) presented SP at the beginning of
treatment, according to Prado (2008) that defined SP if SMI was <55.4 cm2/m2
in males and < 39 cm2/m2 in females.
Results
All
pts concluded the treatment. The acute toxicity profile was analyzed as “less
than” versus “more or equal to” grade 3 CTCAE 4.0. 13 pts (65%) in SP group and
22 pts (39%) in non-SP group presented a toxicity more or equal to grade 3, but
this difference was not statistically significant (p-value 0.25). Overall
survival was analyzed in 65 pts (47 NS and 18 S), excluding pts who finished CT
RT less than 6 months ago (median follow up 41, range 3.4-126.1). Overall
survival was significantly different in non-SP versus SP group (fig 1, p value
0.035). The same difference was notable in N0-N2a pts, suggesting an important
role of SP also in pts with a lower nodal burden and theoretically better
prognosis.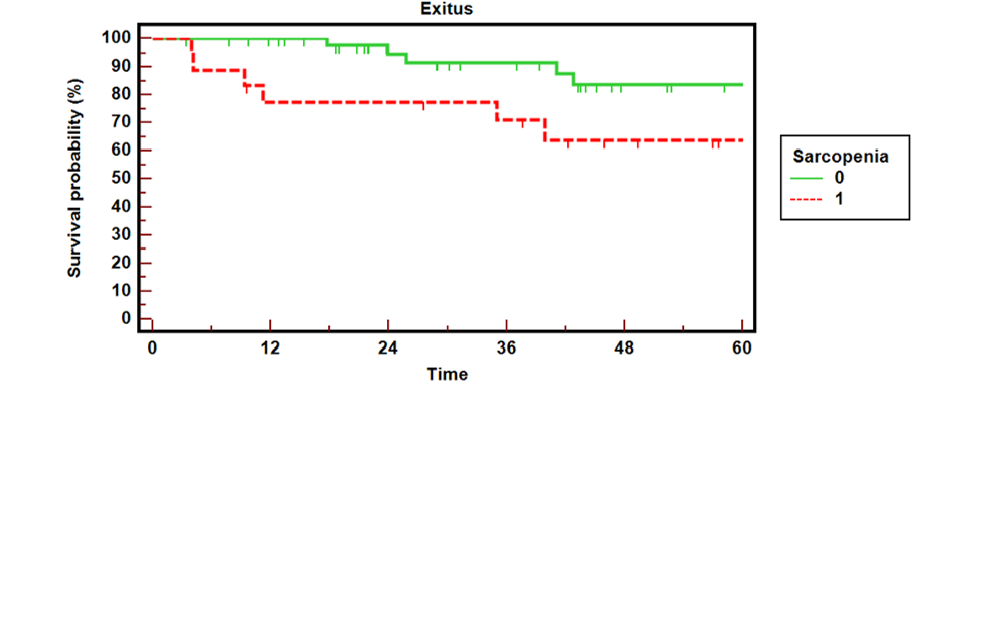
Conclusion
Although
the results are preliminary and limited to a small population, our case series
has the advantage to be very homogeneous in pts and type of treatment
characteristics. In our setting, SP seems to have a crucial impact on overall
survival. Further investigation is necessary to confirm our data and whether SP
is a potentially modifiable risk factor to improve pts outcome.