NLR and PLR ratio as predictive markers of outcomes in head and neck squamous cell carcinoma
Lucrezia Gasparini,
Italy
PO-1073
Abstract
NLR and PLR ratio as predictive markers of outcomes in head and neck squamous cell carcinoma
Authors: Lucrezia Gasparini1, Marzia Borgia1, Marianna Trignani1, Angelo Di Pilla1, Annamaria Porreca2, Marta Di Nicola3, Domenico Genovesi1,4
1SS. Annunziata Hospital, Radiation Oncology Unit, Chieti, Italy; 2D'Annunzio University of Chieti-Pescara, Department of Economics, Pescara, Italy; 3Laboratory of Biostatistics, Department of Medical, Oral and Biotechnological Sciences, Chieti, Italy; 4G. D'Annunzio University, Department of Neuroscience, Imaging and Clinical Sciences, Chieti, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
The identification of biomarkers for oncologic outcomes could guide risk-adapted treatment strategies. High
neutrophil-to-lymphocyte ratio (NLR) is a marker of systemic inflammation and
together with the platelet-to-lymphocyte ratio (PLR) is associated with worse
outcomes in several solid tumours. The aim of this study was to investigate the
prognostic value of NLR and PLR in patients with head and neck squamous cell
carcinoma (HNSCC) treated with primary or adjuvant (chemo)radiotherapy ((C)RT) and
to correlate this parameters to acute toxicity.
Material and Methods
A retrospective analysis of 67 consecutive
patients with HNSCC was performed. Blood samples were obtained within 15 days
before treatment start. Endpoints of interest were overall survival (OS), local
recurrence (LR), distant metastasis (DM), and acute toxicity defined according
to CTCAE v4. Univariate Cox proportional hazards models were used to study
influence of NLR and PLR used both in
the continuum and stratified above and below the median value. To assess
differences in median for NLR and PLR for acute toxicity groups we used the Kruscal
Wallis test. After grouping the patients with toxicity grade G0 and G1, we used
the Mann U-Whitney test to assess differences for the Ratio variables. All
statistical analyses were performed using R statistical software (version
3.1.2.).
Results
Sixty-seven patients with HNSCC were considered.
All patients were candidate for curative RT intent. Primary CRT was
administered in 23 patients (34.3%), primary RT alone in 9 patients (13.4%),
adjuvant (C)RT in 35 (52.3%). Tumours were located in: oral cavity 31.3%, larynx
25.4%, oropharynx 23.9%, parotid 7.5%, ear canal 5.9%, hypopharynx 3%, nasopharynx
3%. Median follow-up was 8 months (range: 1-44 months). The median values of
pre-treatment NLR and PLR were 1.97 (range: 0.07-16.00) and 121.25 (range: 50-285),
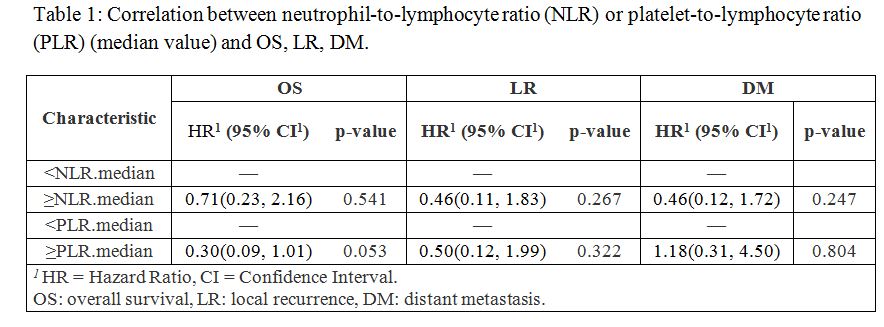
respectively. A statistically significant correlation between OS and a PLR value > of PLR median (p-value=0.053) was found
(Table 1). There were no statistically significant correlations between NLR
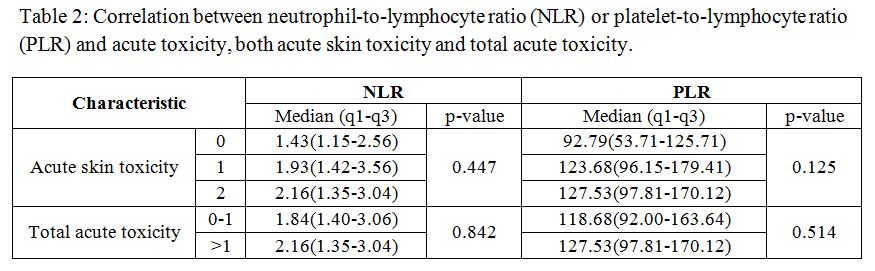
ratio and clinical outcomes (OS, LR, DM). Both NLR and PLR were not associated
with acute toxicity, neither acute cutaneous nor total toxicity (Table 2).
Conclusion
The prognostic significance of NLR and PLR have
been explored in several cancers. In our study a higher pre-treatment PLR in
HNSCC patients resulted predictive of worse OS. The study is still ongoing in
order to validate a larger number of patients and to investigate further readily
available biomarker helpful to improve pre-treatment prognostication and to define
predictive models of risk-stratification.