Resect or Preserve? Comparing treatment strategies in clinically node positive bladder cancer
Martin Swinton,
United Kingdom
PD-0418
Abstract
Resect or Preserve? Comparing treatment strategies in clinically node positive bladder cancer
Authors: Martin Swinton1, Neethu Billy Graham Mariam1, Jean Lin Tan2, Luca Afferi3, Chiara Lonati4, Marco Moshini5, Maurice Lau6, Vijay Ramani6, Vijay Sangar6, Noel Clarke6, Hitesh Mistry7, Thiraviyam Elumalai8, Peter Hoskin1, Ananya Choudhury1
1Christie Hospital, Clinical Oncology, Manchester, United Kingdom; 2University of Manchester, Division of Medical Education, Manchester, United Kingdom; 3Luzerner Kantonsspital, Department of Urology, Lucerne, Switzerland; 4Spedali Civili of Brescia, Department of Urology, Brescia, Italy; 5Urological Research Institute, IRCCS Ospedale San Raffaele, Division of Experimental Oncology/Unit of Urology, Milan, Italy; 6Christie Hospital, Urology, Manchester, United Kingdom; 7Christie Hospital, Pharmacy and Cancer Sciences, Manchester, United Kingdom; 8Addenbrooke's Hospital, Clinical Oncology, Cambridge, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Worldwide there is wide variation in the management of patients with
clinically node positive non-metastatic (cN+M0) bladder cancer. There is a
paucity of high-quality evidence to guide practice. In many European centres, primary management
of fit patients is radical surgery often preceded by platinum-based
chemotherapy. In the UK in contrast, radical radiotherapy (RT) – a
bladder-preserving treatment - is also offered as an alternative treatment to
surgery. To aid clinician and patient decision making, an international
multi-centre retrospective analysis was undertaken to assess clinical outcomes
for cN+M0 bladder cancer receiving radical treatment.
Material and Methods
Data on an international cohort of patients receiving surgery from
2007-2020 for cN+M0 bladder cancer was collated by sending data collection
forms to a number of participating European Medical Centres in France, Italy,
the Netherlands and Russia. Data was collected on a second cohort of cN+M0
bladder patients diagnosed at a large tertiary cancer centre in the UK from
2013-2020. Data was collected on treatment received, clinical outcomes and
patient and tumour factors. Overall survival (OS) was calculated using date of
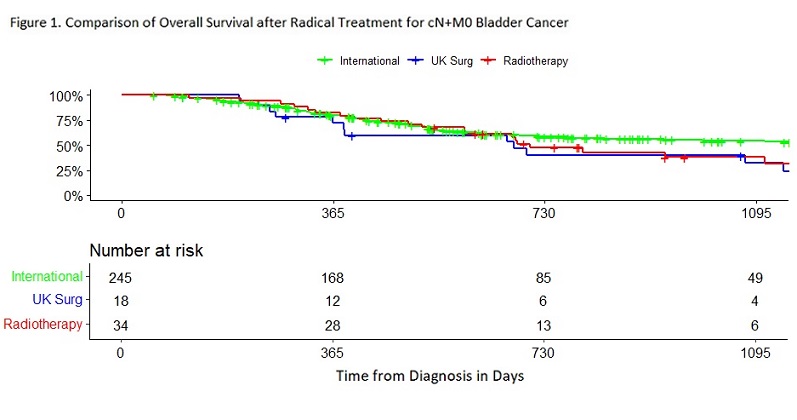
TURBT as t=0. Kaplan-Meier curves for OS were produced for 3 cohorts
‘International’ patients receiving surgery, patients at the UK centre receiving
surgery and UK patients receiving RT. Univariate and multivariate analyses were
performed on the combined cohort to test for an association between nodal
status, T stage, age, receipt of neoadjuvant chemotherapy (NAC) and OS.
Results
245/369 patients with cN+M0 bladder cancer in the International cohort had
OS data for comparison. At the UK centre, 52 patients received radical intent
treatment with either surgery (n=18) or RT (n=34). OS was compared between the 3 cohorts (Figure 1). Median OS
was 3.84 (2.28-NA), 1.85(1.05-NA) and 1.93(1.62-NA) years for the International, UK Surgery and RT groups respectively
however a Log rank test showed no overall survival difference between the 3
cohorts (χ2=3.2, 2 df, p=0.2).
In a univariable analysis OS positively associated with age <70 (HR 0.70
(0.49-0.98) p=0.04) and receiving NAC (HR 0.44 (0.31-0.62) p=0.28) and
negatively associated with T stage 3 or 4 (HR 1.67 (1.14-2.44) p=0.01). Nodal
stage (N1 vs N2/3) and Cohort (International vs UK) showed no statistically
significant association with OS. Only NAC retained a significant association
with OS within a multivariate analysis.
Conclusion
Our retrospective data does not find a significant difference in OS between
cohorts receiving radiotherapy and surgery. Limitations in our data are the
risk of confounders when comparing retrospective cohorts and the smaller number
of RT patients with follow up beyond 3 years. Given the known reduced comorbidities and no operative risk with radiotherapy the data supports a greater use of
radiotherapy in this cohort. Patients across Europe with cN+M0 bladder cancer
should be offered both surgery and radiotherapy as treatment options.