Clinical experiences with online adaptive radiotherapy of vulvar carcinoma
PD-0904
Abstract
Clinical experiences with online adaptive radiotherapy of vulvar carcinoma
Authors: Malene Bak1, Nikolaj Jensen1, Trine Jakobi Nøttrup1, Hanne From Mathiesen1, Henrik Roed1, Maria Emma Eva Sjölin1, Flemming Kjær-Kristoffersen1, Vibeke Nordmark Hansen1, Ivan Richter Vogelius1
1Rigshospitalet, Oncology, Copenhagen, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Vulvar cancer is a
rare malignancy that accounts for ~0.6% of all cancers. Radiotherapy for vulvar
carcinoma is technically challenging due to the target position combined with
common postoperative lymphocele causing anatomical variations. A high burden of
radiation sequelae is observed and locoregional failure is the dominant mode of
failure. Because of these
challenges, vulvar carcinoma became a prioritized patient group for adaptive
radiotherapy in our department. We report on the workflow, rate of adaptation
and dosimetric results for the first eight patients treated for vulvar
carcinoma in our clinic.
Material and Methods
The first adaptive
treatment was performed on January 22, 2021 and eight consecutive patients were
included. This study includes 160 fractions; the adapted plan was chosen for 63
fractions and the scheduled plan for the remainder. Systematic
recording on number of adaptations and causes for not adapting was implemented starting
with patient 4 in order to improve workflow and increase the rate of
adaptation. The recording included reason for not choosing an adaptive plan (if
relevant), adaption time and number of slices edited manually per OAR and
target structures during the adaptive procedure. DVH data from the adapted and scheduled
plans based on setup CBCTs as well as DVH data from the adapted plans based on
verification CBCTs from all 8 patients was analyzed and compared to the planned
dose. The dose covering the hottest 2% of the bladder and rectum was extracted
from DVH. Coverage of the CTV was measured as the minimum
dose covering 95% of the CTV relative to prescription dose. All DVH data was normalized to the reference plans.
Results
The proportions of adapted vs. scheduled plans and the aggregated distributions of the reasons not to adapt are shown in Figure 1A . Dominant
reasons for not adapting were “MD not available for treatment” (15 Fx) and “no significant
dosimetric gain” (13 Fx). The number of slices where OAR and target structures
need editing varied substantially and did not show any clear association with
the proportion of fractions adapted. Median adaption time was 14 minutes and 75th
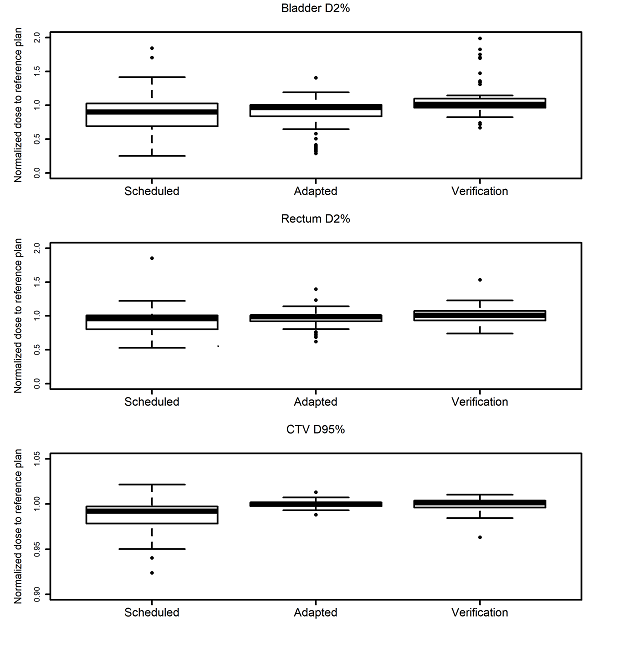
percentile was 17 minutes, cf. Figure 1B. We observed an increase in minimum dose covering 95% of the CTV relative to prescription dose (signrank p<0.0001) which was largely retained at
the verification step, cf. Figure 2. Data on normal tissue doses was more mixed
and didn’t show any gain from adaption. Figure 2 excludes 3 upper outliers
on bladder adapted, 2 upper outliers on bladder verification and 3 lower
outliers on CTV scheduled to improve visualization.
Figure 1:
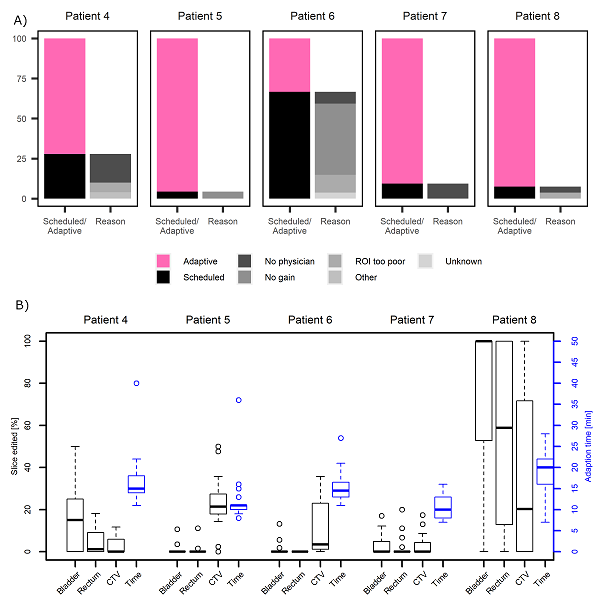
Figure 2:
Conclusion
We
demonstrated a feasible workflow for online adaptive radiotherapy of vulvar
carcinoma. Most fractions can be adapted with some gains in target coverage,
whereas we see no evidence of normal tissue gains. Availability of specialized
MDs for adaptation was the most frequent reason for not adapting, emphasizing
the need for staff training to increase adaption workloads.