Evaluation of a novel CBCT conversion method
PD-0901
Abstract
Evaluation of a novel CBCT conversion method
Authors: Wolfgang Lechner1, Sarah Haupt1, David Kanalas2, Lukas Zimmermann3, Dietmar Georg1
1Medical University of Vienna, Department of Radiation Oncology, Vienna, Austria; 2University of Applied Sciences, Faculty of Engineering, WIener Neustadt, Austria; 3University of Applied Sciences, Faculty of Engineering, Wiener Neustadt, Austria
Show Affiliations
Hide Affiliations
Purpose or Objective
To evaluate a novel implementation of a CBCT
conversion algorithm for dose calculation implemented in RayStation (Development
Version 10B-DTK, RaySearch, Stockholm, Sweden). The algorithm uses deformable
registration to correlate grey scale intensity values with an intensity
conversion function. The algorithm is able to estimate artifacts and create a CBCT
correction map. Additionally, the algorithm uses a stitching technique to
simulate missing tissue outside the field of view (FOV) of the CBCT.
Material and Methods
CBCTs acquired for ten head and neck and ten
gynecological patients were collected and converted using the new algorithm
(CBCTc). A bulk density overriding technique implemented in the same
version of RayStation was used for comparison (CBCTb). The CBCTs and the planning-CT (pCT) were
rigidly registered. Clinical treatment plans, which were optimized on the pCT,
were recalculated on both the CBCTc and the CBCTb. The
resulting dose distributions were analyzed utilizing the MICE toolkit
(NONPIMedical AB Sweden, Umeå) applying local gamma analysis with 1% dose
difference and 1 mm distance to agreement criteria. For both CBCT conversion
methods, the pCT was used as ground truth. Four different dose threshold level were
used for the analysis: 10%, 30%, 50 % and 90%. The 90% threshold was selected to
assess the high dose region around the PTV. A paired student’s t-test was
applied to test the differences in gamma pass rates (GPRs) between the CBCTc
and CBCTb method. A p-value smaller than 0.05 considered
statistically significant.
Results
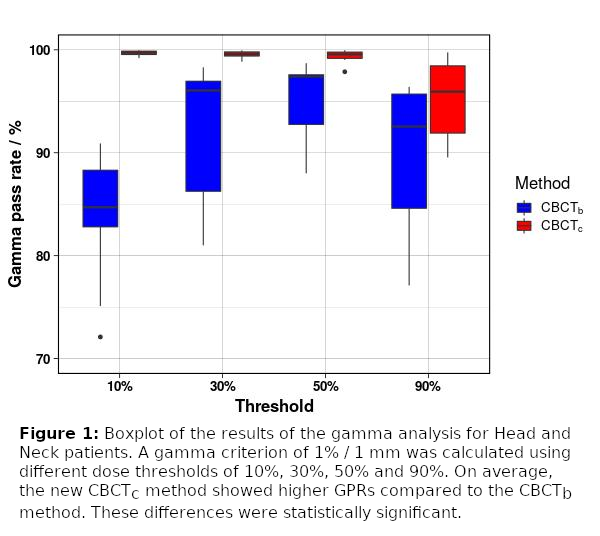
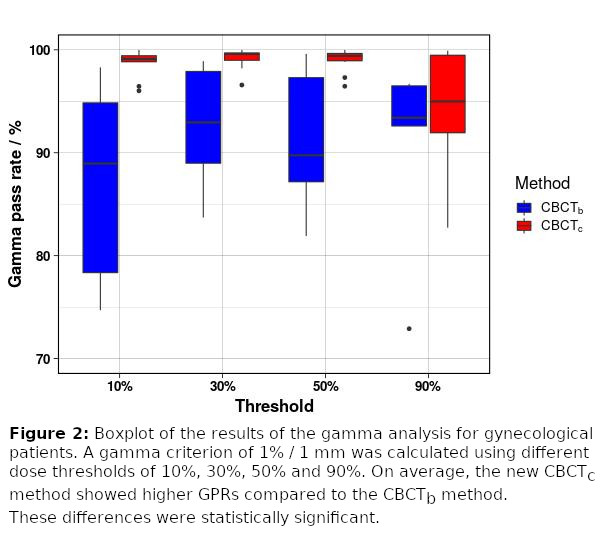
Figure 1 and 2 show box-plots of the GPRs
grouped by conversion method and threshold for the head and neck and gynecological
cases, respectively. On average, the CBCTc method showed GPRs higher
than 95% for all indications and thresholds. The GPRs for the CBCTb
method were systematically lower compared to the CBCTc method. These
differences were also statistically significant for all test cases and
thresholds. The main differences between the dose calculated on the CBCTs and
the pCT were found in regions where weight loss occured frequently or at
air/tissue interfaces, which were also subject to anatomical variations. For
both indications, the stitching technique of the new CBCTc algorithm
provided a reasonable approximation of the missing tissue outside the FOV of
the CBCT. Consequently, better agreement could be achieved between the dose
calculated on the pCT and the CBCTc compared to CBCTb.
Conclusion
The dose distribution
calculated using the new CBCTc method showed excellent agreement
with the pCT based dose calculation, with superior accuracy compared to the
CBCTb method. The main reasons for deviations of the calculated dose
distribution were caused by anatomical variations between the pCT and the
corrected CBCT. The clinical introduction of the novel CBCTc method will
improve the accuracy of the dose estimation in adaptive radiotherapy workflows.