Proton FLASH painting for improved target dose coverage and robustness near risk organs
PD-0900
Abstract
Proton FLASH painting for improved target dose coverage and robustness near risk organs
Authors: Per Poulsen1, Saber Nankali1, Jesper Kallehauge1, Cai Grau1, Morten Høyer1, Brita Singers Sørensen2, Jørgen Petersen3, Anne Vestergaard1
1Aarhus University Hospital, Danish Center for Particle Therapy, Aarhus, Denmark; 2Aarhus University Hospital, Department of Experimental Clinical Oncology, Aarhus, Denmark; 3Aarhus University Hospital, Department of Medical Physics, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
FLASH radiotherapy can
reduce normal tissue damage while maintaining the tumor response. FLASH with
proton beams may be obtained with high energy transmission beams at the cost of
poorer dose conformality. Here, we propose FLASH painting as a method to
deliver proton FLASH therapy with uncompromised dose distributions. FLASH
painting only delivers FLASH dose rates in smaller volumes, where the FLASH
sparing effect is mostly needed. It makes it easier to obtain FLASH dose rates.
This study shows how proton FLASH painting may improve proton therapy of tumors
near the brain stem.
Material and Methods
Proton FLASH painting plans were made for two
patients previously treated with proton therapy for a meningioma (Patient 1) and
an anaplastic oligodendroglioma (Patient 2). The prescribed dose was 59.4Gy in
33 fractions. Since the clinical target volume (CTV) was either overlapping
with or adjacent to the brain stem the CTV dose coverage was compromised in the
clinical treatment plans. The FLASH painting plans had a FLASH painting field
with a single energy layer (~234MeV) that delivered most of the dose in a FLASH
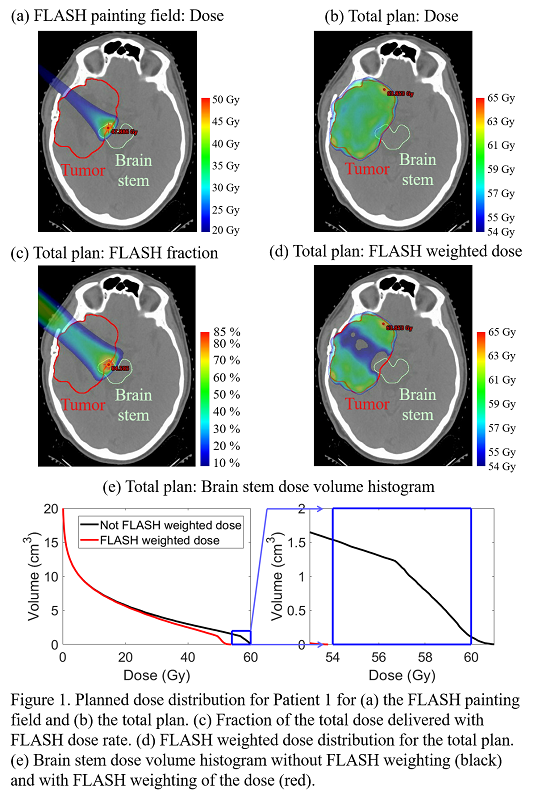
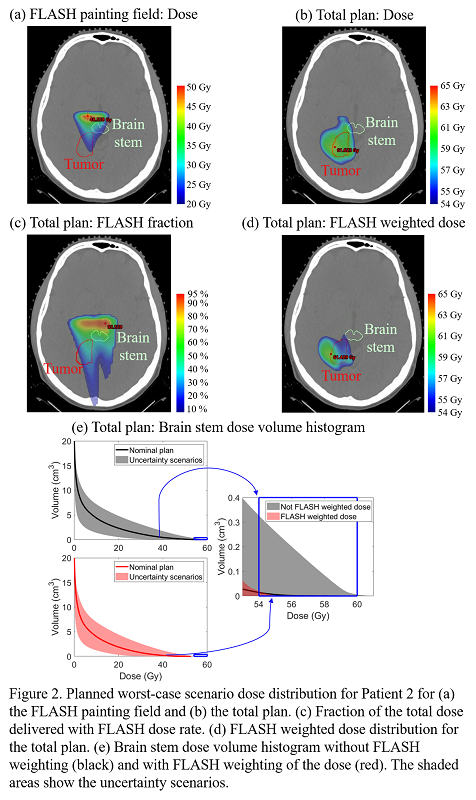
painting volume in or near the brain stem (Figs 1a,2a) and three non-FLASH proton
fields that ensured a uniform CTV dose (Figs 1b,2b). The FLASH painting fields had
~26cm water equivalent beam degrader material in the entrance path to adjust
the Bragg peak to the FLASH painting volume. Delivery of the FLASH painting
fields at a clinical proton facility (ProBeam, Varian Medical Systems) was simulated by assuming 800nA
cyclotron current and the same beam transmission efficiency as measured for the
FLASH painting beam energies at the facility (~5%). The simulated spot
durations were combined with spot specific dose distributions to determine the
dose rate as function of time in each voxel. The FLASH fraction was then
calculated as the fraction of the dose in each voxel that was delivered continuously
with at least 40Gy/s mean dose rate (Figs 1c,2c). Finally, the FLASH weighted
dose to normal tissue was calculated as the dose delivered with FLASH weighted by 80% plus the dose delivered
without FLASH weighted by 100% (i.e by assuming a FLASH sparing effect of 20%) (Figs 1d,2d). The brain stem dose with and
without FLASH weighting was reported to illustrate the potential brain stem
sparing effect of FLASH painting. Plan 1 was made without robust optimization while Plan 2 was optimized and evaluated robustly (±2mm setup, ±3.5% range uncertainties).
Results
Both
FLASH painting plans had full CTV dose coverage (Figs 1b,2b). FLASH painting
reduced the brain stem V54Gy to clinically acceptable levels: from 1.54cm3
to 0.0 cm3 for Plan 1 and from 0.33cm3 to 0.02cm3
for Plan 2 (worst case robustness scenario) (Figs 1d-e,2d-e).
Conclusion
Proton FLASH painting
was proposed as a clinically realizable strategy for proton FLASH treatments
with uncompromised dose distributions. Its ability to cover the CTV while sparing
the brain stem was demonstrated in simulated deliveries of two FLASH painting
plans.