MR-guided lung SBRT: consultation, simulation and treatment delivery in a single day
Miguel A. Palacios,
The Netherlands
OC-0777
Abstract
MR-guided lung SBRT: consultation, simulation and treatment delivery in a single day
Authors: Miguel A. Palacios1, Sonja Verheijen1, Cornelis J.A. Haasbeek1, Ruud de Moes1, Omar Bohoudi1, Famke L. Schneiders1, Anna M.E. Bruynzeel1, Berend J. Slotman1, Frank J. Lagerwaard1, Suresh Senan1
1Amsterdam UMC, VUmc location, de Boelelaan 1117, 1081 HV Amsterdam, Department of Radiation Oncology, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
High precision SBRT delivery is possible using
MR-guided radiotherapy (MRgRT) with real-time intra-fraction tumor motion monitoring.
We implemented a one stop shop (OSS) SBRT service at our department for
patients with lung tumors, and report on the different steps and main findings
during treatment delivery.
Material and Methods
Seven patients with lung cancer underwent an
OSS procedure delivering a single fraction dose of either 30 or 34 Gy. Median GTV was 1.7 cm3 (range 1.3 – 22.9). The
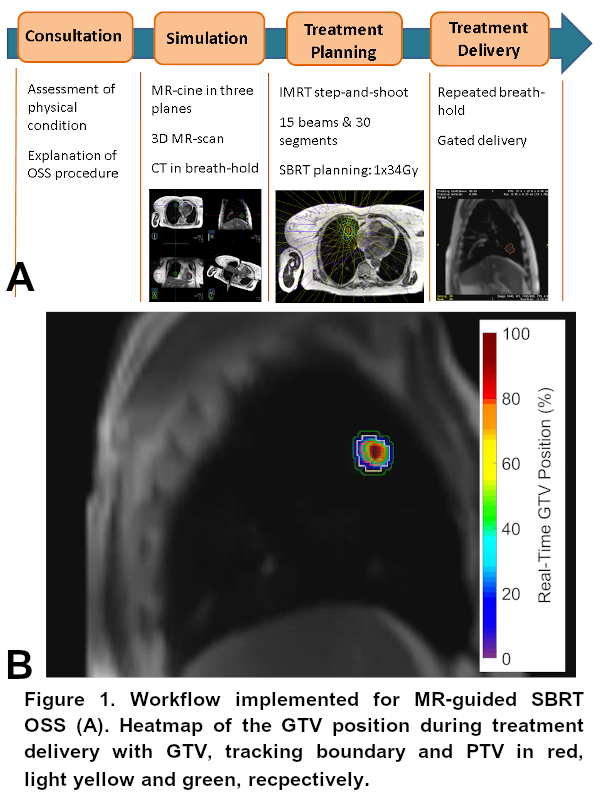
workflow consisted of four consecutive steps: consultation, simulation,
treatment planning and delivery (Figure 1A). The simulation session at the
MR-linac included acquisition of MR-planar image acquisitions in sagittal,
coronal and axial planes, thereby allowing for individualized assessment of
tumor motion for each patient. Tumor contour tracking was also assessed during
the simulation procedure, and the most suitable breath-hold phase for treatment
was identified.
SBRT plans were generated
using step-and-shoot IMRT. A gating boundary of 3mm, and a PTV margin of 5mm around
the GTV, were used to account for system-latency during delivery. SBRT was
delivered during repeated breath-holds, and during gating 10% of the GTV was
permitted to fall outside the tracking boundary before triggering a beam-off. An
analysis of the accuracy of SBRT delivery for each individual patient was
performed to assess the reproducibility of the GTV position inside the PTV, the
effect of system-latency and the duty-cycle.
Results
All 7 patients completed the OSS procedure in a
single day. Five patients were treated in inspiration breath-hold; and 2 in
expiration as this led to a more stable tumor trajectory during breathing.
Figure 1A provides a schematic overview of the OSS workflow. The time needed to
complete the OSS procedure decreased ca. 50% from that of the first
patient and it could be completed in a half-day for the last patients.
Figure 1B shows a heat map indicating the
real-time position of the GTV during treatment delivery for a single patient.
During beam-on, the 3 mm tracking boundary encompassed the GTV by 78.4 – 100%
across all patients, with the corresponding values for the PTV being 94.4 –
100% (2th – 98th percentiles). On average, system-latency
due to gating decisions was involved in 17.4% of the treatment delivery time,
of which 6.2% were directly related to triggering a beam-off after a gating-off
decision. Our use of a tracking boundary inside the PTV minimized the overall
impact of system-latency on GTV coverage to only -0.3% on average. Duty-cycle efficiency
during treatment delivery ranged from 31.1 – 64.7%.
Conclusion
An MR-linac OSS SBRT service for lung
tumors was successfully implemented, using a dedicated simulation procedure and
gated breath-hold delivery. All patients completed same-day SBRT delivery and
it can now be completed in a half-day. Use of a tracking boundary of 3mm inside
the PTV minimized the impact of system-latency on GTV coverage.