Integrated beam angle optimization in IMRT autoplanning for lung cancer
Kristine Fjellanger,
Norway
PD-0731
Abstract
Integrated beam angle optimization in IMRT autoplanning for lung cancer
Authors: Kristine Fjellanger1,2, Liv Bolstad Hysing1,2, Ben J. M. Heijmen3, Helge Egil Seime Pettersen1, Inger Marie Sandvik1, Turid Husevåg Sulen1, Sebastiaan Breedveld3, Linda Rossi3
1Haukeland University Hospital, Department of Oncology and Medical Physics, Bergen, Norway; 2University of Bergen, Institute of Physics and Technology, Bergen, Norway; 3Erasmus University Medical Center, Department of Radiotherapy, Rotterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
IMRT with fixed beams is a much applied technique for treatment of
locally advanced non-small cell lung cancer (LA-NSCLC), to avoid large lung
volumes receiving low dose. However, manually selecting the optimal beam
configuration for each patient is a challenging task due to large anatomical
variations between patients. The aims of this study were to use automated IMRT planning
with integrated beam angle optimization (BAO) to 1) enhance plan quality
compared to manual planning, 2) investigate patterns in selected beam
configurations and 3) investigate the impact of the applied number of beams on plan
quality.
Material and Methods
26 LA-NSCLC patients were prospectively included. The prescribed dose
was 60-70 Gy in 2 Gy fractions. All patients had a clinical 6-beam IMRT plan
(CLIN), manually created by an expert planner. Using a novel in-house developed
system for automated multi-criterial IMRT planning with integrated BAO, clinically
deliverable plans with 4, 6 and 8 optimized beams were created for each patient
(AUTO). Candidate beam
angles were 140°-40° for right-sided tumors and 320°-220° for left-sided tumors
(5° spacing). Dose-volume parameters related to toxicity and patterns of selected
beam angles were compared for 6-beam CLIN and AUTO plans. 4-, 6- and 8-beam AUTO
plans were mutually compared. The Wilcoxon signed-rank test (p ≤ 0.05) was used for statistical
testing.
Results
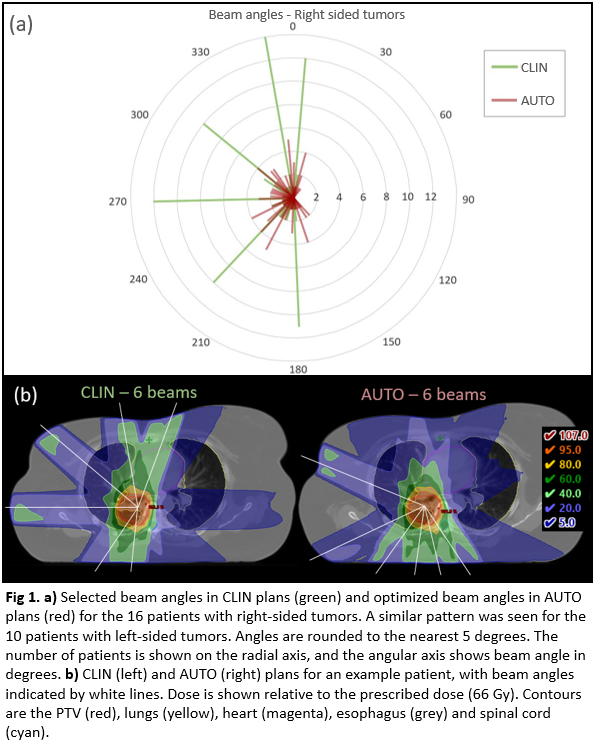
In the CLIN plans, there were mainly small variations from the planning
beam template and all patients had opposing beams in the AP direction. In contrast, the angles in the 6-beam
AUTO plans were spread out across the candidate beam space, demonstrating more patient-specific
selection (Fig. 1). The resulting AUTO plans were dosimetrically clearly superior to the
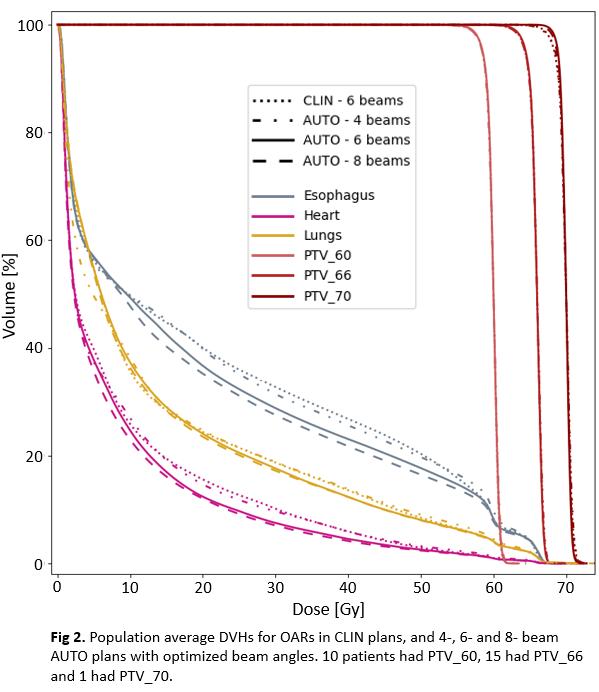
CLIN plans (Fig. 2). While
PTV coverage and lung dose were similar, the median heart Dmean was
reduced from 9.0 Gy to 8.1 Gy (p = 0.02), median esophagus Dmean
from 20.3 Gy to 18.5 Gy (p = 0.02), median heart V30Gy from 11.0% to
6.2% (p = 0.002) and median esophagus V20Gy from 38.4% to 36.8% (p =
0.008). Fig. 1b shows large differences in selected beams between 6-beam CLIN
and AUTO plans for an example patient, with clear impact on heart and esophagus
sparing. Dosimetric QA at the linac proved deliverability of the 6-beam AUTO
plans. Overall,
increasing the number of optimized beams improved OAR sparing, with a larger
impact of going from 4 to 6 than from 6 to 8 (Fig. 2).
Conclusion
Selected beam angles have a significant impact on IMRT plan quality for LA-NSCLC
patients. Automated planning with integrated computerized BAO showed a great
potential for enhanced OAR sparing compared to planning with manually selected
angles. Dosimetric
implications of increasing or reducing the number of beams were
patient-specific, but overall, increasing the number of beams improved OAR
sparing. Autoplanning allows for generation of several plans with different
numbers of optimized beams to select the optimal number for each individual
patient.