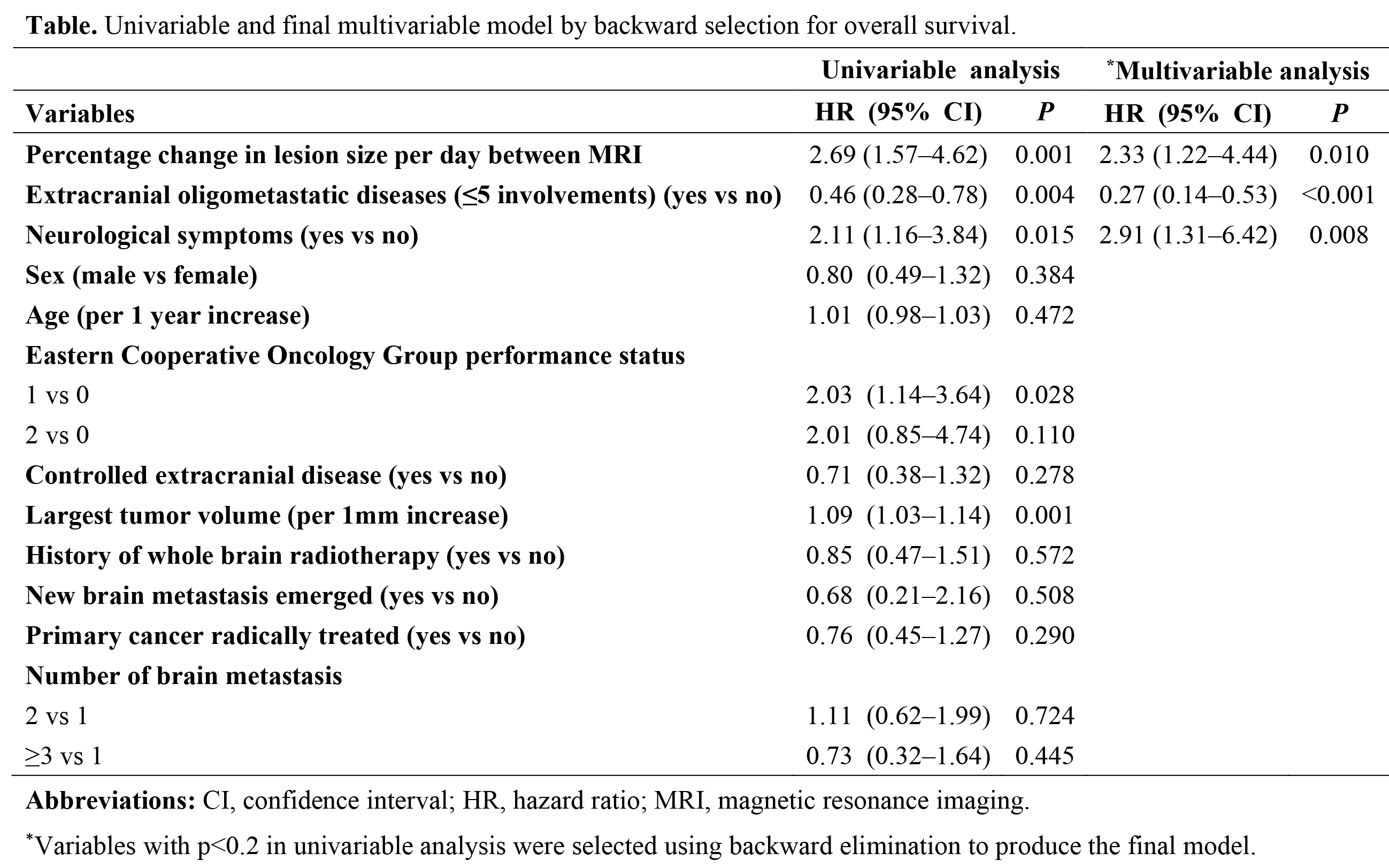
Total
85 patients were included, and 67 (79%) of them had positive growth in the size
of brain metastasis. The median follow-up duration was 20 months (interquartile
range [IQR] 10-34 months). Overall survival for the whole cohort was 17 months
(95% confidence intervals [CI], 12–22 months). We developed the prognostic model
based on the most important predictors of OS: percentage change in lesion size
per day between the diagnostic and stereotactic MRI (hazard ratios [HR] of ≥1%
vs <1%, 2.33; 95% confidence interval [CI], 1.22–4.44), extracranial
oligometastatic diseases (≤5 involvements) (HR, 0.27; 95% CI, 0.14–0.53), and
the presence of neurological symptoms (HR, 2.91; 95% CI, 1.31–6.42). For our
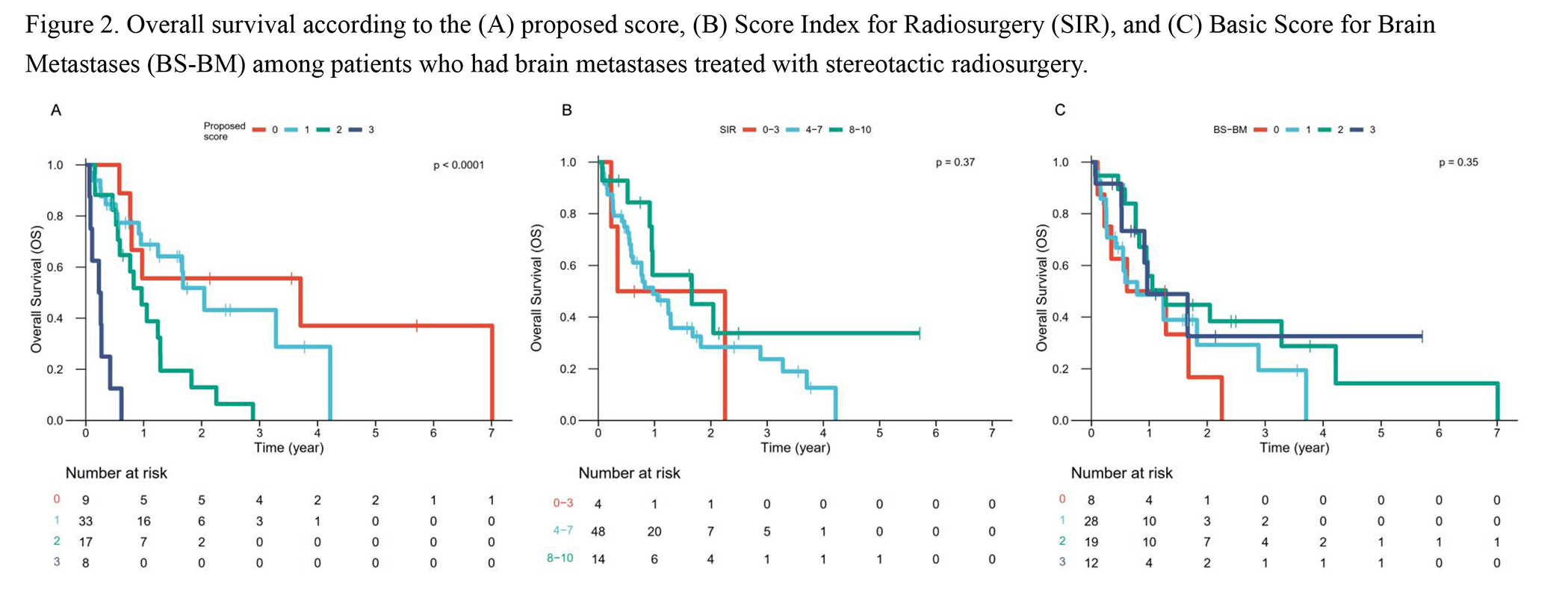
model, patients with scores 0, 1, 2, and 3 had a median OS of 3.7 (95% CI 0.8–not reached [NR]),
2.0 (95% CI 1.2–NR), 1.0 (95% CI 0.6–1.8), and 0.2 (95% CI 0.1–NR) years,
respectively. Pairwise comparisons using Log-Rank tests showed statistically different
survival except between score 0 and 1. The
optimism-corrected c-index for the proposed model, SIR, and BS-BM were 0.681
(95% CI, 0.594–0.773), 0.560 (95% CI, 0.450–0.662), and 0.559 (95% CI,
0.461–0.657), respectively.